Introduction
Ulcerative Colitis (UC) is an idiopathic chronic Inflammatory
Bowel Disease (IBD) caused by a dysregulated mucosal immune
response to the intestinal microflora in genetically predisposed
hosts [1]. IBD and Human Immunodeficiency Virus (HIV) infection
may coexist in the same individual [2]. We report the first case of
a patient with HIV infection and diagnosis of UC with subsequent
evidence of endoscopic polypoid lesions healed after Highly Active Antiretroviral Therapy (HAART), in absence of anti-inflammatory drugs.
Case report
A 56-years-old caucasian man with Parkinson’s disease in neurological follow-up was admitted to the Emergency Department in
July 2019 for several episodes of rectal bleeding. A rectal examination showed an internal haemorrhoidal congestion, requiring anti-fibrinolytic therapy with only partial and transitory clinical improvement. He performed a colonoscopy that showed in the recto sigmoid area a swollen hyperemic mucosa and multiple fibrin-coated
ulcers. Histological findings were suggestive for ischemic colitis.
In September 2019 he had a recurrence of rectal bleeding. For
this reason he was hospitalized and he underwent classical Milligan-Morgan procedure for hemorrhoidectomy. Thereafter, the
patient presented diarrhea with bleeding and abdominal pain.
Due to clinical worsening, he repeated a colonoscopy with evidence of multiple mucosal ulcerations in the sigmoid colon and
in the rectum with histological features of ulcerative colitis. The
patient was treated with oral/topical mesalazine and methylpredinosolone with clinical response but symptoms worsened after
discontinuation of steroids.
In January 2021 the patient was admitted to our Department
presenting rectal bleeding and iron deficiency anemia. Based on
the severity of the endoscopic lesions and on the steroid dependence, we planned an endoscopic re-evaluation and screening
for biologic therapy. Moreover he performed an intravenous iron
supplementation.
His chest X-ray and electrocardiogram were normal and Quantiferon-TB Gold test was negative. Stool examination was negative
for bacterial and parasitic organism. Diagnostic markers of viral
hepatitis and antinuclear antibodies were normal. Unexpectedly,
the patient resulted positive to human immunodeficiency virus
(HIV) test with high viral load (quantitative HIV RNA 72.131 copies/ml). The number of CD4+ lymphocites, in the acute phase,
was 850/ μl while CD8+ lymphocites were 4714/ μl. He underwent
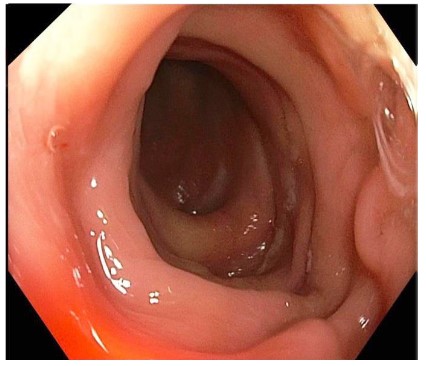
endoscopic evaluation that showed normal sigmoid mucosa but
multiple nodular elements with mucosal hyperemia and erosions
in the rectum (Figure 1).
Histological evaluation found a lymphocyte infiltrate consisting
of a prevalence of small-sized T lymphocytes (CD3+ and CD5+)
with a mixture of CD4+ and CD8 + lymphocytes with a small count
of B+ lymphocytes (CD 20+). In the samples there were no elements referable to chronic IBD and no evidence of Kaposi’s sarcoma. At immunohistochemistry and citofluorimetry no signs of
monoclonality or images suggestive for lymphoma were seen.
Therefore, after ruling out opportunistic infections, on April
2021 he started Highly Active Antiretroviral Therapy (HAART)
based on bictegravir, emtricitabine and tenofovir alafenamide
combination in order to reduce the viral load and to increase
CD4+ cell count. Treatment initiation was associated with a better clinical outcome. On September 2021 a new colonoscopy was
performed. The mucosa appeared macroscopically normal from
the rectum to the cecum, no particular lesions were found on the
mucosal surface (Figure 2). The patient was in good general condition. In October 2021 the viral load was significantly decreased
with immune reconstitution of CD4+ T-cells.
Discussion
We report the first case of endoscopic polypoid lesions referable to HIV infection undergoing complete healing after treatment with highly active antiretroviral therapy (HAART).
Our patient had a short history of symptoms and signs of UC.
HIV infection was occasionally found and no risk factors could be
identified. Following HAART, endoscopic and histologic lesions
were healed. In the pathophysiology of IBD, leukocytes play an
important role, in particular CD4+ T lymphocytes are thought to
be crucial in the inflammatory processes [3,5]. Patients with human immunodeficiency virus infection often present depletion
of the number of CD4+ lymphocytes because of viral replication,
resulting in a wide range of clinical consequences especially opportunistic infections [4,5]. Our case confirmed the reports of literature that showed improvement of symptoms in concomitant
HIV infection in IBD patients, thus supporting a key role of CD4+
cells in the pathogenesis and clinical course of IBD. Viazis et all
[5] conducted a retrospective matched case-control study comparing the course of IBD in HIV patients with a matched group of
IBD seronegative patients. Their study showed HIV infection reduces the relapse rate in IBD patients because of the lower CD4+
counts seen in these patients. In our case, fortunately, the patient
remained free of opportunistic infections commonly associated
with HIV. On the contrary, Liebowitz et all [6] reported a patient
with long-standing ulcerative colitis who developed HIV infection and his clinical conditions were worsened by opportunistic
infections (Kaposi’s sarcoma, syphilis, and oral candidiasis) probably due to also previous treatment with steroids. An interesting
study conducted by Lori Fantry et all. [7] compared colonoscopy
findings in HIV-infected men and women from an urban United
States cohort to non-HIV-infected demonstrating that the former
subjects were less likely to have any polyp (hyperplastic, adenomatous or adenocarcinoma), neoplastic lesion, adenoma compared to the latter and that the lesions were mostly found in the
proximal colon. Instead, in our case, we found polypoid lesions in
the rectum with lymphocyte T infiltrate (CD3+, CD5+, CD4+, CD8+)
and a small count of CD20+ B lymphocytes. Furthermore a prior
study [8] found that the use of HAART was associated with a significantly lower odds of adenomatous lesions on colonoscopy (the
reasons for these findings are unknown) while in our case HAART
induced complete endoscopic remission of polypoid lesions.
Conclusion
In conclusion, our case is the first one showing HAART induced
complete clinical-endoscopic remission, in absence of anti-inflammatory drugs. However, further studies are needed to confirm
HIV-associated gut inflammation.
Declarations
No funding was received to assist with the preparation of this
manuscript. The authors have no competing interests to declare
that are relevant to the content of this article. Informed consent
was obtained from the patient. The participant has consented to
the submission of the case report to the journal.
References
- Ungaro R, Mehandru S, Allen PB, Peyrin-Biroulet L, Colombel JF.
Ulcerative colitis. Lancet. 2017; 389: 1756-1770.
- Sharpstone DR, Duggal A, Gazzard BG. Inflammatory bowel disease in individuals seropositive for the human immunodeficiency
virus. Eur J Gastroenterol Hepatol. 1996; 8: 575-578.
- Himmel ME, Hardenberg G, Piccirillo CA, Steiner TS, Levings MK.
The role of T-regulatory cells and Toll-like receptors in the pathogenesis of human inflammatory bowel disease. Immunology. 2008;
125: 145-153
- Sierra S, Kupfer B, Kaiser R. Basics of the virology of HIV-1 and its
replication. J Clin Virol. 2005; 34: 233-244.
- Viazis N, Vlachogiannakos J, Georgiou O, Rodias M, Georgiadis D,
et al. Course of inflammatory bowel disease in patients infected
with human immunodeficiency virus. Inflamm Bowel Dis. 2010;
16: 507-511.
- Liebowitz D, McShane D. Nonspecific chronic inflammatory bowel
disease and AIDS. J Clin Gastroenterol. 1986; 8: 66-68.
- Fantry LE, Nowak RG, Fisher LH, Cullen NR, Yimgang DP, et al. Colonoscopy Findings in HIV-Infected Men and Women from an Urban
U.S. Cohort Compared with Non-HIV-Infected Men and Women.
AIDS Res Hum Retroviruses. 2016; 32: 860-867.
- Bini EJ, Green B, Poles MA. Screening colonoscopy for the detection of neoplastic lesions in asymptomatic HIV-infected subjects.
Gut. 2009; 58: 1129-1134.