Introduction
Patients who have been treated with re irradiation for recurrent glioma reported survival benefits [1,2]. Gliomas of Grade III
and IV, based on the WHO classification, are generally treated according to the Stupp protocol [3]. The procedure of brain tumors
classification is completed since June 2016 with the additional
use of molecular testing [4]. After a total or subtotal resection a
primary radiation dose of 60Gy in 30 fractions is indicated. For
patients with glioblastoma of WHO Grade IV confirmed from molecular testing, a chemotherapy with Temozolomide is indicated
simultaneously to radiotherapy while for maintenance a Temozolomide of 12 cycles is scheduled. Maintenance is suggested to be
scheduled with Temozolomide of 6 cycles for patients with tumor
of Grade III.
The median survival for patients with glioblastoma after
following a primary radio chemotherapy is 12 months. For
tumors of Grade III the prognosis depends on molecular and
histopathological characteristics. After progression the optimal
treatment for a pretreated glioma is yet unclear. Local re-irradiation has been established as a feasible option for recurrent
glioma patients. Although re-irradiation is accompanied with the
concern about the risks of toxicity and radio necrosis risk, many
studies have shown that it is a safe option and may effectively
increase the overall survival in selected patients [2]. However, the
radiation dose and its fractionation it is still uncertain and is the
subject of several ongoing trials. The fractionation of radiation
dose might affect the effectiveness of re-irradiation in survival
and quality of patient’s life.
Methodology
Between 2012 and 2020, 35 patients with recurrent gliomas
were re-irradiated with VMAT (volumetric modulated arc therapy).
Nine patients were diagnosed with astrocytoma and twenty six
patients with glioblastoma multiforme. Patient demographics
are presented in Table 1. For first treatment patients received
subtotal or total resection with adjuvant radiotherapy of 60Gy
and 30 days in VMAT technique with simultaneous chemotherapy
(Temozolomide). After recurrence, resection has been repeated
followed by re-irradiation of 45Gy in 15 fractions (BED biological
effective dose 56Gy) in VMAT technique. The median interval
between the first radiotherapy and the re-irradiation was 6
months.
Table 1: Patient Demographics.
| Characteristics |
Number |
| Total Number of Patients |
35 |
| Sex |
|
| Male |
|
| Female |
|
| Age |
|
| Median 49 (range: 22-74) |
|
| ≤ 49 |
18 |
| > 49 |
17 |
| 1st radiation dose |
60 Gy |
| 2nd radiation dose |
45 Gy |
For all the patients the following outcomes were assessed: 1)
overall survival; 2) progression-free survival. Survival was evaluated using Kaplan-Meier analysis. Furthermore, the Karnofsky Performance Scale score (Yates et. al. 1980) was also used as another
predictor of survival. Karnofsky Performance Scale score quantifies the patient abilities by measuring its level of activity and support needed. All statistical analyses were carried out using SPSS
software. Overall Survival (OS) was defined as the time from the
first radiation treatment or the re-irradiation to death.
Results
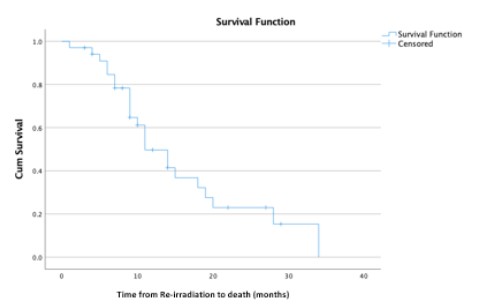
Figure 1 shows the progression free survival for patients after
first radiation and after re-irradiation. After the end of re-irradiation the progression free survival was 6 months (3.8-8 months)
while after the end of first radiation was 13 months (8-17.9
months). The overall survival after combining radiation with re-irradiation is also presented in Figure 1. A combination of radiation and re-irradiation achieved a median overall survival of 42
months (95% confidence interval, 29-54 months). Figure 2 shows
the patient survival after the end of re-irradiation. After the end
of re-irradiation the median overall survival was 11 months (95%
confidence interval, 7-14 months).
Discussion
Recurrent Glioblastoma WHO IV is associated with a median
overall survival of less than a year [5] and the majority of patients
have profound tumor-related symptoms. The results of this study
suggest that re-irradiation may prolong the overall survival. This
is in agreement with the results found by Fetcko et al. [6] who reported in a systematic review that in high-grade gliomas a median
overall survival is 20.19 months (9-65 months) and progression
free survival is 5.42 months (3-16 months). The small number of
sample used in the current study might limit the evidence of our
findings.
Conclusion
Re-irradiation of recurrent glioma patients with VMAT technique might prolong survival rates.
References
- Minniti G, Niyazi M, Alongi F, Navarria P, Belka C. Current status
and recent advances in reirradiation of glioblastoma. Radiat Oncol.
2021; 16: 36.
- Combs SE, Thilmann C, Edler L, Debus J, Schulz-Ertner D. Efficacy of
fractionated stereotactic reirradiation in recurrent gliomas: long-term results in 172 patients treated in a single institution. Journal
of clinical oncology. 2005; 23: 8863-8869.
- Stupp R, Mason WP, Van Den Bent MJ, Weller M, Fisher B, et al.
Radiotherapy plus concomitant and adjuvant temozolomide for
glioblastoma. New England journal of medicine. 2005; 352: 987-
996.
- Louis, DN, Perry A, Reifenberger G, Von Deimling A, Figarella-Branger D, et al. The 2016 World Health Organization classification of
tumors of the central nervous system: a summary. Actaneuropathologica. 206; 131: 803-820.
- Easaw JC, Mason WP, Perry J, Laperrière N, Eisenstat DD, et al.
Canadian recommendations for the treatment of recurrent or
progressive glioblastoma multiforme. Current oncology. 2011; 18:
126-36.
- Fetcko K, Lukas RV, Watson GA, Zhang L, Dey M. Survival and complications of stereotactic radio surgery: A systematic review of
stereotactic radiosurgery for newly diagnosed and recurrent highgrade gliomas. Medicine (Baltimore). 2017; 96: e8293.