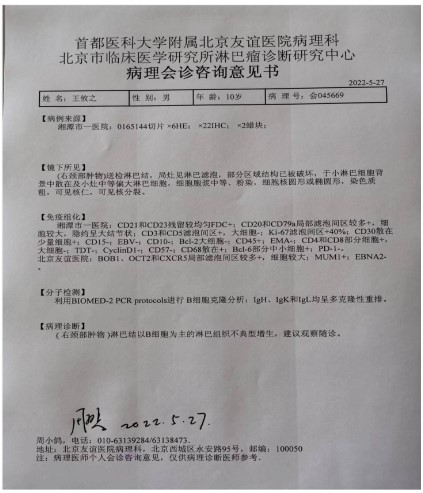
Case presentation
A 10-year-old man was admitted to our hospital for a year after
the discovery of a tumor in his neck. The boy had a history of eczema, a highly sensitive constitution, and a long history of taking
the anti-immune drug tacrolimus.
Physical examination: an egg-sized lymph node can be touched on the right side of the neck, about 4 × 3 cm in size, medium,
no tenderness, mobility can be, with no adhesions.
Color ultrasound: multiple nodules can be seen subcutaneously, some of which are a very low echo, oval, clear borders, enveloping, and internal echoes are under-clear.
Excision biopsy as seen by the naked eye: a round tumor, 4.5 ×
size 3 × 4 cm, gray, solid, local bleeding, delicate texture.
Microscopic: lymph nodes (right neck mass)are tested, lymph
follicles are seen on focal spots, some regional structures have
been destroyed, scattered in the background of small lymph node
cells and medium-sized lymphocytes in small foci, the cytoplasm
is medium, molten, nucleus is round or oval, coarse chromatin,
the nucleoli are visible, the nuclear division is visible.
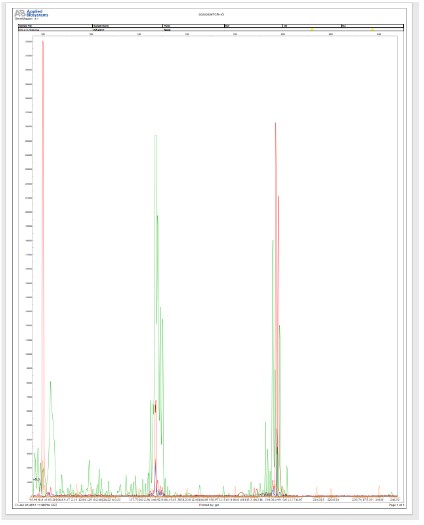
Immunohistochemistry: CD21 and CD3 residues are more uniform, FDC+; CD20 and CD79a local follicular zone more+, the cells
are relatively large, vaguely large nodular; CD3 and CD5 follicular
region +, large cells -; Ki-67 interveolar zone +40%; CD30 scattered
in a small number of cells+; CD15-; EBV-; CD10-; Bcl-2 large cells-;
CD45+; EMA-; CD4 and CD8 partial cells +, large cells -; TDT-; CyclinD1-; CD57-; CD68scattered+; Bcl-6 part of small cells +; PD-1-.
BOB1, OCT2 and CXCR5 have more local follicular intervenorial
regions and larger cells; MUM1+; EBNA2-.
Diagnosis: Proliferative lesions (resembling nodular lymphocyte-predominant Hodgkin lymphoma).
Discussion
At the molecular level, tacrolimus is clearly useful for accumulation in cells using binding to a cellular protein (FKBP12). The
FKBP12-tacrolimus complex specifically binds to and inhibits calcinurin, which inhibits the calcium-dependent signaling pathways
produced in T cells, thus preventing transcription of discontinuous lymphogenemic genes [1]. This drug is a highly immunosuppressive drug, and its activity has been confirmed in vitro and
in vivo experiments. This drug inhibits the production of cytotoxic
lymphocytes that form the main transplant rejection effect. This
drug inhibits the activation of T cells and the proliferative effect
of T helper cells dependent on B cells. It also inhibits the production of lymphoid factors such as interleukin-2, interleukin-3, and
γ-interferon and the expression of interleukin-2 receptors. At the
molecular level, the effects of the drug appear to be produced by
binding to a cellular protein (FKBP), which also causes the compound to accumulate between cells. In in vivo tests, the drug has
been shown to be effective for liver and kidney transplantation
[2].
Clinical experiments show that it has a good effect on heart,
lung, intestine, and bone marrow transplantation [1,2,23,24].
FK506 also plays an active role in the treatment of Atopic Dermatitis (AD), Systemic Lupus Erythematosus (SLE), autoimmune
eye diseases, myasthenia gravis, and other autoimmune diseases
[25-27].
Atypical lymphoid hyperplasia refers to other malignant lesions
in the lymph nodes that cannot be diagnosed as malignant lymphoma or lymphoid reticular tissue, and atypical hyperplasia of
lymphoid tissue is benign and malignant lymphoid hyperplasia lesions that have not yet been determined, or lympho proliferative lesions between typical hyperplasia and typical lymphoma [3]. At
present, it can be classified as atypical hyperplasia of lymphoid
tissue: lymphatic follicles have more than 5 hyperplasias of the
same size and shape; Fusion and consistent hyperplasia of more
than 1/3 of the lymph nodes in the paracortical region; Vascular
immunoblastic lymphadenopathy; Proliferation of mucosal-associated lymphoid tissue in the focal consistent mononucleoid B-cell
region; Extraosseous isolated plasma cell tumors; Pseudosymphima outside the node [4]. If the reactivity of lymphoid tissue is
insufficient for the diagnostic criteria of lymphoma, but cannot be
classified as reactive hyperplasia, in this case, it can be called atypical hyperplasia of lymphoid tissue, and its clinical significance is
that such cases should be closely followed up because they may
develop lymphoma.
According to the WHO classification, typical nodules are necessary for the diagnosis of this tumor. NLPHL may have diffuse
areas [5,20]. CD20 staining is helpful for discrimination, Recognize
nodules in diffuse areas. Looking for popcorn cells in nodules is
diagnostic NLPHL is very important. There are many or few tumor
cells. In this case, the tumor cells are rare and the tumor cells
are relatively small, Misdiagnosis is easier when young. Follicular
dendritic cells and germinal center cells in tumor cell body, It is
difficult to identify in size, and the identification is mainly based
on typical cell morphology and immunohistochemistry [6,7].
Based on previous case reports and literature studies, we have
found that a small number of patients do have cancer after longterm treatment with tacrolimus, and tumorigenesis is likely [8].
Therefore, it is disturbing that few articles advocating the use
of topical or internal tacrolimus in patients with high sensitivity
take into account that this topical immune agent may increase
the risk of squamous cell carcinoma as well as tumors of the blood
system, however, for a new drug that has not yet stood the test
of time, its risks need to be considered very carefully, and the
drug can be used for the skin or mucous membranes of the skin
or mucous membranes that can be widely treated with topical
steroids [9]. In earlier studies, we found that the use of immunosuppressant’s such as glucocorticoids resulted in an increased risk
of squamous cell carcinoma, basal cell carcinoma, and Hodgkin
lymphoma, so surveillance biases were unlikely to explain the observed associations. The incidence of skin cancer and non-Hodgkin lymphoma has increased worldwide [10-13]. This suggests
that these malignant tumors may have a common cause, perhaps
related to the heavy use of immunosuppressant’s [14].
We found that previous animal experiments have demonstrated that immune agents in mice can indeed lead to the development of lymphatic system tumors, including cyclosporine and
tacrolimus [15]. Prior studies with ciclosporin have shown that
topical application of the drug in the DMBA/TPA model inhibited
tumour formation in mice, while systemic immune suppression
with ciclosporin accelerated carcinogenesis [16,17]. There is evidence that this differential outcome is related tothe differential
effects of ciclosporin, i.e. local anti-inflammatory action and systemic immune suppression [18]. The preclinical topical carcinogenicity studies with tacrolimus, which have resulted in a significant
lymphoma signal in mice have shown that systemic immune suppression can be achieved with a protocol of daily application of
the 0.1% tacrolimus ointment formulation[19].
Sánchez-Pérez J et al demonstrated that nowadays there
doesn’t exist scientific evidence of an increase of skin cancer, lymphomas or systemic immune suppression in those patients that
use or have used topical tacrolimus. Nevertheless, it is not possible to exclude the possibility that there appear cutaneous and/
or systemic long-term side effects [21,22].
Conclusion
In this case, our diagnosis suggests that Proliferative lesions
(resembling nodular lymphocyte-predominant Hodgkin lymphoma) is indirectly and probably caused by long-term use of the immune drug tacrolimus in pediatric patients with a hypersensitivity
system. Early diagnosis can improve the survival of patients, who
are prone to relapse, but have a longer survival even if they relapse.
Declarations
Consent to participation and ethical approval: This article is
a case report, hence, this research was exempt from the ethical
approval statement and the necessity of informed consent.
Data and materials accessibility
The datasets used in this investigation may be found in The
First People’s Hospital of Xiangtan City.
Competing interests: There are no competing interests declared by the authors.
Funding: There was no particular funding for this research but
as part of the author's work.
Contributions of Authors: Shixuan Peng was in charge of the
report's overall execution and manuscript writing, while Yongjun
Wu was in charge of collecting the data and diagnosing the disease.
Acknowledgements: We thank The First People’s Hospital of
Xiangtan City which offered a platform in this case.
References
- Venkataramanan R, Swaminathan A, Prasad T, Jain A, Zuckerman
S, et al. Clinical pharmacokinetics of tacrolimus. Clin Pharmacokinet.1995; 29: 404-430.
- Schutte-Nutgen K, Tholking G, Suwelack B, Reuter S. Tacrolimus-Pharmacokinetic Considerations for Clinicians. Curr Drug Metab.
2018; 19: 342-350.
- Schroer KR, Franssila KO. Atypical hyperplasia of lymph nodes: a
follow-up study. Cancer.1979; 44: 1155-1163.
- Good DJ, Gascoyne RD. Atypical lymphoid hyperplasia mimicking
lymphoma. Hematol Oncol Clin North Am. 2009; 23: 729-745.
- Cazzola M. Introduction to a review series: the 2016 revision of
the WHO classification of tumors of hematopoietic and lymphoid
tissues. Blood. 2016; 127: 2361-2364.
- Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, et al. The
2016 revision to the World Health Organization classification of
myeloid neoplasms and acute leukemia. Blood. 2016; 127: 2391-
2405.
- Sabattini E, Bacci F, Sagramoso C, Pileri SA. WHO classification of
tumours of haematopoietic and lymphoid tissues in 2008: an overview. Pathologica. 2010; 102: 83-87.
- Cho M, Puma I, Nguyen D, Schut R, Glesne L. Development of
Kaposi’s sarcoma in an AIDS patient after treatment with topical
tacrolimus. J Am Acad Dermatol. 2004; 50: 149-150.
- Bunker CB, Neill S, Staughton RC. Topical tacrolimus, genital lichen
sclerosus, and risk of squamous cell carcinoma. Arch Dermatol.
2004; 140: 1169.
- Hjalgrim H, Frisch M, Begtrup K, Melbye M. Marked increase in incidence of non-Hodgkin’s lymphoma among young peoplein Denmark during 1943-1989. Ugeskr Laeger. 1997; 159: 2999-3002.
- Lopes FCPS, Sleiman MG, Sebastian K, Bogucka R, Jacobs EA, et
al. UV Exposure and the Risk of Cutaneous Melanoma in Skin of
Color: A Systematic Review. JAMA Dermatol. 2021; 157: 213-219.
- Willenbrink TJ, Ruiz ES, Cornejo CM, Schmults CD, Arron ST, et al.
Field cancerization: Definition, epidemiology, risk factors, and outcomes. J Am Acad Dermatol. 2020; 83: 709-717.
- Karagas MR, Greenberg ER, Spencer SK, Stukel TA, Mott LA. Increase in incidence rates of basal cell and squamous cell skin cancer in New Hampshire, USA. New Hampshire Skin Cancer Study
Group. Int J Cancer. 1999; 81: 555-559.
- Sørensen HT, Mellemkjaer L, Nielsen GL, Baron JA, Olsen JH, et al.
Skin cancers and non-hodgkin lymphoma among users of systemic
glucocorticoids: a population-based cohort study. J Natl Cancer
Inst. 2004; 96: 709-711.
- Lübbe J, Sorg O. Tacrolimus ointment and skin carcinogenesis in
the DMBA/TPA model in mice. Br J Dermatol. 2004; 151: 1275-
1276.
- Venuti A, Salani D, Manni V, Poggiali F, Bagnato A. Expression of
endothelin 1 and endothelin A receptor in HPV-associated cervical
carcinoma: new potential targets for anticancer therapy. FASEB J.
2000; 14: 2277-2283.
- Bagnato A, Cirilli A, Salani D, Simeone P, Muller A, et al. Growth inhibition of cervix carcinoma cells in vivo by endothelin A receptor
blockade. Cancer Res. 2002; 62: 6381-6384.
- Bonifati C, Mussi A, Carducci M, Pittarello A, D’Auria L, et al. Endothelin-1 levels are increased in sera and lesional skin extracts of
psoriatic patients and correlate with disease severity. Acta Derm
Venereo. l1998; 78: 22-26.
- Bagnato A, Venuti A, Di Castro V, Marcante ML. Identification of
the ETA receptor subtype that mediates endothelin induced autocrine proliferation of normal human keratinocytes. Biochem Biophys Res Commun. 1995; 209: 80-86.
- Sabattini E, Bacci F, Sagramoso C, Pileri SA. WHO classification of
tumours of haematopoietic and lymphoid tissues in 2008: an overview. Pathologica. 2010; 102: 83-87.
- Connors JM, Cozen W, Steidl C, Carbone A, Hoppe RT, et al. Hodgkin lymphoma. Nat Rev Dis Primers. 2020; 6: 61.
- Sánchez-Pérez J. Safety information for tacrolimus: present and
future. Actas Dermosifiliogr. 2008; 2: 19-25.
- Yu M, Liu M, Zhang W, Ming Y. Pharmacokinetics, Pharmacodynamics and Pharmacogenetics of Tacrolimus in Kidney Transplantation. Curr Drug Metab. 2018; 19: 513-522.
- Staatz CE, Tett SE. Clinical pharmacokinetics and pharmacodynamics of tacrolimus in solid organ transplantation. Clin Pharmacokinet. 2004; 43: 623-653
- Fleischmann R, Iqbal I, Stern RL. Tacrolimus in rheumatoid arthritis. Expert Opin Pharmacother. 2006; 7: 91-98.
- Zhai J, Gu J, Yuan J, Chen J. Tacrolimus in the treatment of ocular
diseases. Bio Drugs. 2011; 25: 89-103.
- Kim YH, Shin HY, Kim SM. Long-Term Safety and Efficacy of Tacrolimus in Myasthenia Gravis. Yonsei Med J. 2019; 60: 633-639.