Introduction
A liver abscess is a pyogenic cavity in the liver parenchyma produced by bacterial invasion of liver tissue [1]. The occurrence of
liver abscesses is worldwide, with substantial variability between
nations. Pyogenic liver abscess occurred in 4.1 cases per 100,000
people in the United States [2]. According to a population retrospective research, the incidence of liver abscess in China was 8.9
cases per 100,000 persons, with pyogenic liver abscess accounting
for the great majority of cases [3]. It is also much higher than in
Canada, Denmark, and the United Kingdom [4-6]. Pyogenic liver
abscess is a specific type of septic disease in which infection of the
liver parenchyma can be fatal. However, conventional treatments
tend to be lengthy and costly and have many adverse effects.
Through a review of clinical cases, we confirmed an emerging
therapy, which is an oral liquid prepared by extracting medicinal
plant components for symptomatic and anti-infective treatment,
that quickly heals liver abscesses, directly solves inflammation
problems, consolidates the root, and repairs the disease, and is it
shortens the treatment process. It reduces both unpleasant reactions and negative effects.
Case report
A 48-year-old lady with a 10-day history of fever (40.1°C) and
liver pain presented to a district hospital. Anti-infection therapy
was given at the local hospital, but the results were disappointing.
Then she was admitted to our hospital with a «liver abscess». She
suffered from «tuberculosis» as a child and was already healed.
She has no family history of genetic or infectious diseases.
A physical examination on admission revealed that the abdomen was modest pressure pain without other signs or symptoms.
Her laboratory evaluation showed a white blood cell count of 4.9
x 109/L, a neutrophil count of 12.22 x 109/L, and procalcitonin of
0.230 ng/ml.
Her liver function showed glutamate transaminase of 57 U/L,
glutamate transaminase of 64 U/L, glutamate dehydrogenase of
11.6 U/L, γ-Glutamyl trans peptidase of 137 U/L, alkaline phosphatase of 170 U/L, albumin of 33.4 g/L. G test, GM test, and
blood culture were negative.
Based on a preliminary diagnosis of pyogenic liver abscess, the
patient was given the treatment for liver protection and anti-infection for the time being. When no obvious improvement occurred after 4-day antibiotic treatment, but the patient still had intermittent fever. Then, we gave symptomatic remedies to clear away
the liver fire, disperse stagnated liver qi for relieving qi stagnation,
and clear heat and detoxify medicinal plant oral solution.
The active ingredients were extracted from 12 g of Cortex LyciiRadici, 12 g of Paeoniae Radix Alba, 18 g of Herba Artemisia, 9 g
of Poria, 9 g of Radix Rehmanniae Praeparatae, 20 g of Viburnum
biflorum, 9 g of Fructus forsythia, 12 g of Lophatherum gracile
Brongn, 15 g of RhizomaPhragmites, and 3 g of Radix Glycyrrhizae.
After the treatment of 2 days, the patient had no further fever. A
week later, the medicinal plant composition was changed to add
12 g of Moutan Cortex. The combination of liver protection and
anti-infection medication was maintained. After half a month, the
indices had returned to normal. After a month, the recipe was
changed based on the condition, and 9 g of Fructus Schis andrae
was added to create a blend of 12 medicinal plants. 48 days later,
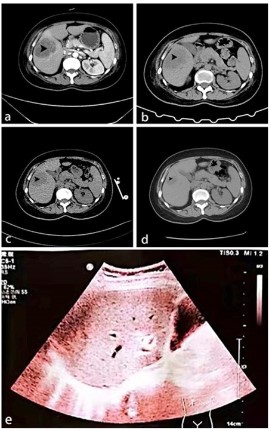
the abdominal ultrasonography showed that the lesions had completely disappeared (Figure 1).
Clinical application discussion
Pyogenic liver abscess is a common clinical inflammatory disease of the liver. The clinical signs and symptoms of pyogenic
liver abscess are nonspecific and usually present with chills and
hyperthermia, discomfort in the liver area, and enlargement of
the liver. It is usually diagnosed by imaging, with ultrasonography and computed tomography confirming the diagnosis in more
than 90% of cases [1,7]. In this clinical case, it was excluded other
causes of liver abscess based on the patient’s past medical history and biological findings. Pyogenic liver abscesses are usually
treated with high-dose antibiotics, which have a long course, high
cost, and a range of side effects. Moreover, the optimal application of antibiotics is based on drug sensitivity results, but blood
cultures of some patients often fail to detect sensitive bacteria,
so the empirical use of antibiotics is not targeted, and in some
areas with limited resources, response persisted[8, 9]. Furthermore, some research centers advocate surgical drainage of liver
abscesses larger than 5 cm, however, repeated drainage has been
reported to worsen the infection, and severe cases can result in
death due to sepsis and systemic failure.
According to certain research, there is a 26% chance of developing postoperative sepsis [10,11].
Based on the poor anti-infective effect of conventional antibiotics, our biggest advantage in this case of the liver abscess was to
avoid the traditional surgical method of imaging-guided drainage
and to treat the patient with medicinal plants to clear the liver
and fire, regulate qi, and clear heat, and detoxify the liver. After 48
days of treatment, imaging showed that the patient’s lesions had
been completely absorbed and disappeared. There were no further symptoms such as fever or liver discomfort, which achieved
a clinical cure and allowed the patient to avoid invasive surgery’s
pain and potential risks.
In clinical practice, the medicinal plant ingredients can effectively prevent or eliminate the formation of pus walls and at the
same time promote the phagocytosis of white blood cells, resulting in the absorption and dissipation of inflammation and abscesses. Treatment of liver abscesses with the extracted botanical
components can significantly improve the clinical symptoms of
patients and reduce the total duration of treatment. This method
plays a direct role in the treatment process of liver abscesses by
resolving inflammation, fixing the root cause, and repairing the
disease, with fewer adverse reactions and side effects during the
treatment process.
Conclusion
Medicinal plant extracts can be an emerging therapeutic approach for treating liver abscesses. They have great potential in
combating liver abscesses and even liver disease safely and reliably and avoiding invasive manipulations. We can apply it as a
novel therapeutic material in a larger target population for further exploration, and combine it with its molecular technology
to make mechanisms of medicinal plant chemical components
be continuously improved, thus providing a solid clinical basis for
new drug development.
Declarations
Acknowledgment: This study was supported by the National Key Research and Development Program of China (No.
2021YFC2301800).
Conflict of interest: The authors declare no conflicts of interest.
Author contributions: Kai Wang and Zhaohui Wang contributed to the clinical study design and protocol development. Kai
Wang performed the configuration of extracts. Zhaohui Wang and
Jingwen Wang performed a clinical investigation of patients, collected, reviewed, analyzed, and interpreted the data, and wrote
the draft manuscript. Ying Zhang, Huihui Liu, and Yuchen Fan analyzed and processed the imaging and followed up with the patient. All authors collected and analyzed data and contributed to
the revision of the manuscript.
Ethics statement: Written informed consent was obtained
from the patient for the publication of any potentially identifiable
images or data included in this article.
References
- Lardière-Deguelte S, Ragot E, Amroun K, Piardi T, Dokmak S, et al.
Hepatic abscess: Diagnosis and management. J Visc Surg. 2015;
152: 231-243.
- Meddings L, Myers RP, Hubbard J, Shaheen AA, Laupland KB, et al.
A population-based study of pyogenic liver abscesses in the United
States: incidence, mortality, and temporal trends. Am J Gastroenterol. 2010; 105: 117-24.
- Tian LT, Yao K, Zhang XY, Zhang ZD, Liang Y-J, et al. Liver abscesses
in adult patients with and without diabetes mellitus: ananalys is
of the clinical characteristics, features of the causative Pathogens,
outcomes and predictors of fatality: are port based on a large population, retrospective study in China. Clin Microbiol Infect. 2012;
18: E314-30.
- Jepsen P, Vilstrup H, Schønheyder HC, Sørensen HT, et al. A nationwide study of the incidence and 30-day mortality rate of pyogenic liver abscess in Denmark, 1977-2002. Aliment Pharmacol
Ther. 2005; 21: 1185-1188.
- Mohsen AH, Green ST, Read RC, McKendrick MW, et al. Liver abscess in adults: ten years experience in a UK centre. Qjm. 2002; 95:
797-802.
- Hansen PS, Schønheyder HC. Pyogenic hepatic abscess. A 10-year
population-based retro spective study. Apmis. 1998; 106: 396-402.
- Pang TC, Fung T, Samra J, Hugh TJ, Smith RC, et al. Pyogenic liver
abscess: an audit of 10 years’ experience. World J Gastroenterol.
201; 17: 1622-1630.
- Khim G, Em S, Mo S, Townell N. Liver abscess: diagnostic and management issues found in the low resource setting. Br Med Bull.
2019; 132: 45-52.
- Lo JZ, Leow JJ, Ng PL, Lee HQ, Mohd Noor NA, et al. Predictors of
therapy failure in a series of 741 adult pyogenic liver abscesses. J
Hepatobiliary Pancreat Sci. 2015; 22: 156-165.
- Chou FF, Sheen-Chen SM, Chen YS, et al., Single and multiple pyogenic liver abscesses: clinical course, etiology, and results of treatment. World J Surg. 1997; 21: 384-388.
- Thomas J, Turner SR, Nelson RC, Paulson EK, et al. Post procedure
sepsis in imaging-guided per cutaneous hepatic abscess drainage:
how often does it occur? AJR Am J Roentgenol. 2006; 186: 1419-
1422.