Introduction
Weak uterine contractions during cesarean section are the
most common cause of Postpartum Hemorrhage (PPH) [1], accounting for 70-80% of cases, with a progressive increase [2-4],
For weak uterine contractions in addition to the first use of uterine
contraction agents, when they are ineffective, surgical treatment
needs to be used as early as possible [5,6]. The B-Lynch method
of uterine loop suturing and intrauterine balloons Intrauterine
Balloons (IUB) are relatively easy and commonly used methods
to stop bleeding, but in recent years complications associated
with uterine loop suturing have been reported, such as myometrial damage necrosis, catastrophic uterine rupture in mid to late
pregnancy, uterine adhesions, secondary infertility, etc., causing
pelvic and abdominal adhesions and bringing about a significantly
higher incidence of complications [7-12]. Recently, in our hospital,
due to intraoperative uterine contraction weakness after using
circumferential suturing caused partial ischemic necrosis of the
uterus and secondary infection, the patient was treated conservatively for up to 6 months and eventually the ischemic necrotic
tissue of the uterus gradually returned to normal and the infection was controlled, the clinical data of this patient combined with
literature review is reported below.
Case information
Female, 26 years old, primigravida. The pregnancy was terminated by cesarean section due to social factors, intraoperatively
the uterus was weakly contracted after placental spontaneous
abruption, and she was given 20 U of contractin, 2 ml of motherwort uterine body injection, 0. 2 mg of ergometrine maleate
injection drip, 2 layers of myometrium were continuously sutured with barbed sutures, and 1 layer of plasma myometrium was
continuously sutured with barbed sutures, the uterus was still
weakly contracted like a sack, continuous massage of the uterus
was ineffective, she was given 0. 9% NS+ The uterus contraction
was still not improved, the uterus was quickly delivered outside
the abdominal cavity, and the uterus was circumferentially sutured and tied with 1-0 absorbable thread in the non-vascular
area of the broad ligament of the parametrium for 3 times with
an interval distance of about 5.0 cm, the uterus was observed to
be circumferential in shape, the uterus was normal in color, and
no blood was oozing from the suture eyes, and the uterus was
placed into the The pelvic cavity was explored and the abdomen
was closed after the uterine incision suture was free of blood and
the bilateral adnexa were free of abnormalities. On postoperative day 4, he developed fever and was treated with ceftazidime
+ ornidazole. On postoperative day 11, he was still febrile, and the culture result of vaginal secretion suggested Escherichia coli
(+). Moxifloxacin + Ornidazole triple anti-infection. On the 13th
postoperative day, fever was still present, and in order to be alert
to potential fungal infection, the medication was adjusted to the
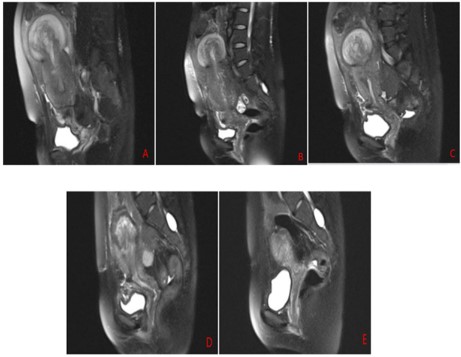
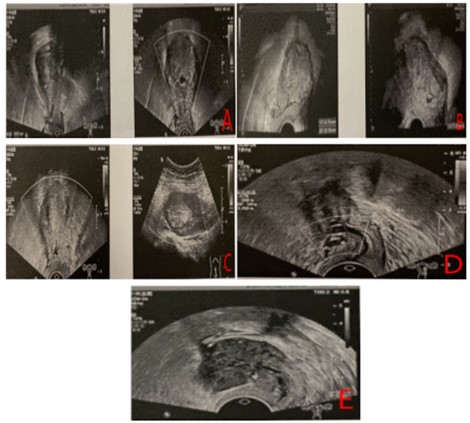
combination of meropenem + voriconazole anti-infective treatment. No fever was observed after the 15th postoperative day. Relevant postoperative ancillary tests are shown in Figures 1, 2
and 3 below.
Table 1: Postoperative antibiotic use in this case.
| Time (post-operative) |
Fever |
Antibiotics |
| the same day |
not |
Cefuroxime sodium |
| 4 d |
have |
Ceftazidime + Ornidazole |
| 11 d |
have |
Ceftazidime + Ornidazole + Levofloxacin |
| 12 d |
have |
Meropenem + Moxifloxacin + Ornidazole |
| 13 d |
have |
Meropenem + voriconazole |
| 15 d |
not |
Meropenem + voriconazole |
Table 2: Post-operative review of the mother in this case.
| Time
(post-operative) |
Magnetic resonance results |
Time
(post-operative) |
Color ultrasound results |
| 11 d |
The uterus is enlarged and the wall thickened, with
fascicular changes seen in the fundic-body junction area,
which is poorly defined. |
34 d |
The uterine body measures approximately 98 x 89 x 59 mm, and
an inhomogeneous echogenic mass measuring approximately 65
x 66 x 45 mm is seen in the uterine cavity. |
| 15 d |
The uterus was enlarged, wall thickened, and fasciculated
changes were seen in the fundic-body junction area,
which was reduced from the previous subserosal cystic
lesion within the uterus. |
48 d |
The uterine body is approximately 78 x 89 x 55 mm in size, and
an inhomogeneous hyperechoic mass of 55 x 77 x 50 mm in size
is seen in the uterine cavity. |
| 25 d |
The uterus was enlarged and wall thickened, with
fascicular changes seen in the fundus-body junction area,
64 mm in diameter; the cystic lesion was reduced from
the previous fundus and body of the uterus. |
67 d |
The size of the uterine body was about 67 x 61 x 37 mm and the
size of the inhomogeneous hyperechoic mass was seen in the
uterine cavity about 51 x 47 x 29 mm. |
| 59 d |
The uterus is slightly enlarged and a round-like cystic long
T2 signal of approximately 44X39X6 2mm is seen at the
base of the uterus, which is reduced from the previous
cystic lesion at the base of the uterus. |
125 d |
The size of the uterine body is about 31 x 39 x 35 m, and a mixed
echogenic area with a range of about 28 x 13 m is seen in the
middle and lower part of the uterine cavity. |
| 188 d |
The uterus was not abnormal in size or morphology,
and the bottom wall was seen to be 12m m in diameter
isosignal; it was significantly smaller than the previous
fundal uterine lesion. |
188 d |
The size of the uterine body was about 34 x 37 x 27 mm, and an
area of 11 x 6 mm inhomogeneous echogenicity was seen within
the myometrium at the lower anterior wall incision. |
Discussion
Uterine contraction weakness refers to the weakness of uterine contraction, as the most common cause of postpartum hemorrhage, and is also an indication for uterine compression suture [4], the basis of this suture technique used in surgery is from
the British scholar B-Lynch proposed in 1997 [13], it belongs to a
kind of uterine body compression suture, through the compression of the uterine cavity, reduce the volume of the uterine cavity
to achieve the purpose of hemostasis, mainly used for bleeding
caused by contraction weakness of the uterine body part, currently based on this suture technique has been derived from surgical
sutures used in different ranges and with different advantages
and disadvantages [14,15], such as Haymen modification of the
B-Lynch suture technique, Cho square suture (patch suture, multi-square pressure suture), Hwu suture (patch suture, multi-square
pressure suture), Hwu suture (parallel vertical compression suture of the lower uterine segment), etc. In this case, the patient
developed partial ischemic necrosis of the myometrium and secondary infection after circumferential binding suture of the uterus, and the early antibiotics used failed to control the infection
effectively. Therefore, in similar rare cases when infection cannot
be effectively controlled with conventional antibiotics, whether
early prophylactic use of antifungal drugs would bring unexpected anti-infective effects and perhaps better improve the patient's
postoperative recovery, and avoid the occurrence of infection.
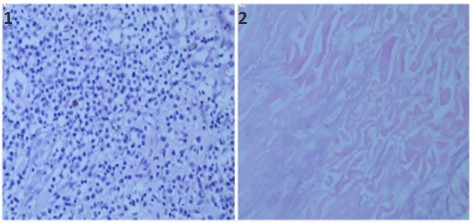
After postoperative imaging data, hysteroscopy and pathological
examination all suggest the presence of defective necrotic lesions
in the uterus and the presence of infection in the uterine cavity,
whether hysterectomy must be performed to resolve the symptoms of ischemic necrosis and infection when imaging and related ancillary examinations and clinical symptoms suggest the presence of ischemic necrosis and co-infection, after the availability
of hysterectomy guidelines [4], it is still necessary to For patients
who are primiparous or have high fertility requirements, and
whose clinical symptoms have gradually decreased after surgery
and whose lesions have gradually decreased in size and normalized on relevant ancillary tests, continued conservative treatment
under close monitoring is also a better option. Ischemic necrosis
of the uterus complicated by infection as one of the complications
after cricothyrotomy [4], this patient as a rare clinical case, after
ischemic necrosis of the uterus and secondary infection through
up to six months of conservative treatment, not only the infection was controlled, ischemic necrosis of the uterus lesion also
gradually shrunk and returned to normal, although avoiding hysterectomy, but for our clinical treatment of such cases brings reflections, for intraoperative uterus due to Although hysterectomy
was avoided, it brings reflections on our clinical treatment of such
cases. For patients who underwent uterine cricothyrotomy due to
weak intraoperative contraction, more attention should be paid
to postoperative condition monitoring, clinical treatment, and clinical care to achieve early monitoring, early treatment, and early
management to facilitate postoperative recovery.
References
- Ma HW, Liu XH. Changes in the etiological composition of postpartum hemorrhage and countermeasures. Journal of Practical Obstetrics and Gynecology. 20 21; 37: 165-168.
- Bateman BT, Berman MF, Riley LE, Leffert LR. The epidemiology of
postpartum hemorrhage in a large, nationwide sample of deliveries. Anesth Analg. 2011; 31: 89.
- Kramer MS, Berg C, Abenhaim H, et al. lncidence, risk factors, and
temporal trends in severe postpartum hemorrhage. Am J Obstet
Gynecol. 2013; 209: 449.
- Joseph KS, Rouleau J, Kramer MS, Young DC, Liston RM, et al. Investigation of an increase in postpartum haenordlage in Canada.
BJOG. 2007; 114: 751.
- Obstetrics and Gynecology Group of the Chinese Medical Association, Obstetrics and Gynecology Branch. Guidelines for the prevention and management of postpartum hemorrhage. Chinese Journal of Obstetrics and Gynecology. 2014; 49: 641-646.
- Liu XH, He R. Prevention and management of postpartum hemorrhage. Chinese Journal of Practical Gynecology and Obstetrics.
2020; 36: 123-126.
- Cotieb AG, Pandipati S, Davis KM, Gibbs RS. Uerine necrosis:a complication of uterine compression sutures. Obstet Gynecol. 2008;
112: 429-431.
- Ibrahim MI, Raafat TA. Elaithy MI. Risk of postpartum uterine synechiae following uterine compression suturing during pospartum
hemorrhage. Aust N z J Ohmtet Gynacol. 2013; 53: 37-45
- Jiang L, Yang F, Yang F. A cease repont of complications fllowing a
combination of modulated B-lynch and Hwu sutures in postpartum hemorrhage: haematocele in the uterine cavity, hemoperitoneum and swelling and nupture of the fallopian tube. J Obstet
Gynaccol. 2019; 39: 115-117.
- Pechtor K. Richards B. Paterson H. Antenatal eatastophic uterine
rupture at 32 weeks of gestation after previous B-Lynch suture.
BJOG. 2010; 117: 889-891.
- An GH, Ryu HM, Kim MIY, Han JY, Chung JH, et al. Outcomes of
subsequent pregnancies after uterine compression sutures for
postpartum hemorrhage. Obstet Gynecol. 2013; 122: 565-570.
- Date s, Murthy B, Maglum A. Pot B-lynch uterine rupture: ease report and review of literature. J Obstet Gymeeol. 2014; 64: 362-363.
- B-Lynch C, Coker A, Lawal AH, Abu J, Cowen MJ. The B-Lynch surgical technique for the control of massive post-partum hemorrhage:
an alternative to hysterectomy? Five cases re- ported. Br J Obstet
Gynaecol.1997; 104: 372-375.
- Kayem G, Kurinczuk JJ, Alfirevic Z, Spark P, Brocklehurst P, et al.
Specific second-line therapies for postpartum hemorrhage: a national cohort study. BJOG. 2011; 118: 856-864.
- Zhang GH, Shen XY, Cui WH. Etiology finding, joint management
and prevention and control of disseminated intravascular coagulation in secondary uterine contractile bleeding. Chinese Journal of
Practical Gynecology and Obstetrics. 2022; 38: 161-164.