Introduction
Approximately 90% of thyroid cancers are differentiated thyroid carcinoma, which include follicular thyroid carcinoma, papillary thyroid carcinoma. The primary treatment modalities are
surgery, selective postoperative radioiodine therapy and thyroid
stimulating hormone suppressive therapy [1]. In this case report,
a complicated medical condition of a patient with a history of invasive follicular carcinoma have been discussed.
Case report
A 24-year-old female with a history of widely invasive Follicular
Thyroid Carcinoma (FTC), including intraluminal involvement of
the Right Internal Jugular Vein (RIJV). The patient had two surgeries and three doses of radioiodine (RAI) therapy.
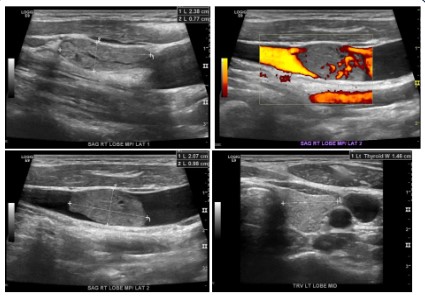
The patient visited the General Practitioner (GP) Clinic for regular check-up, her physician noticed a lump on her neck. Ultrasound (US) soft tissue/Thyroid scan was performed to rule out the
suspected thyroid goitre. As a result, (Figure 1) shows follicular
thyroid carcinoma involving soft tissue was found revealing a 5 cm tumour with positive lymphatic invasion, extensive angioinvasion, positive perineural invasion, although without extrathyroidal extension. Carcinoma extended to less than 0.1 cm from the
external surface. One of the eight (1/8) lymph node was positive
for metastases.
Following the detection of thyroid carcinoma, the patient had
her first surgery for total thyroidectomy with the excision of the
right internal jugular vein as well as excision of lymph nodes in addition to the excision of the right lateral neck tissue. After surgery,
the patient had a radioiodine ablation therapy with approximately
106.7 mCi dose of 131I.
During follow up after one year of the first surgery, the Whole-Body Scan (WBS) was negative, but the stimulated Thyroglobulin
(TG) was greater than 150 (after a baseline value of TG 7.6 was
recorded). A month later, TG was 14.5 with negative Computed
Tomography (CT) neck and negative Positron Emission Tomography/ Computed Tomography (PET/CT) scan.
Two months later, the patient noticed a lump in the anterior
neck and more recently appreciated growth in the size of the lump
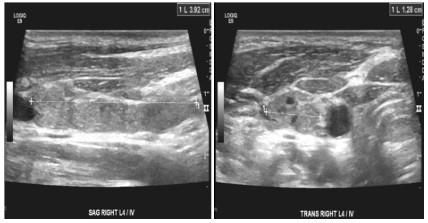
over the couple of months. Mapping Ultrasound (US) neck and
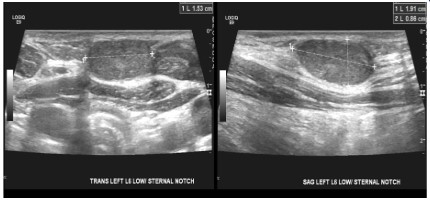
Fine Needle Aspiration (FNA) was done, in figure 2 FNA showed
the presence of metastatic follicular thyroid carcinoma in right level intrajugular vein lymph node and left sternal notch (Figure 3)
while US neck revealed 2.6 cm RT thyroid bed mass partially engulfing RIJV with associated intraluminal tumour thrombosis with
80% stenosis, Few bilateral metastatic cervical lymph node also
noted with the largest in LT level VI 1.5 cm.
CT neck showed 2 cm mass at the level of thoracic inlet suggestive of tumour along the surgical tract. Seven months later, TG
level increased to 61.6. Then the patient underwent for the second surgery, the patient had a reoperation of right modified neck
dissection and right central neck dissection as well as resection of
the right internal jugular vein. The pathology report indicated that
the presences of FTC in the central neck (5 mm) in aggregation,
FTC involving right internal jugular vein and infiltrating the skeletal muscle and RT lateral neck wall.
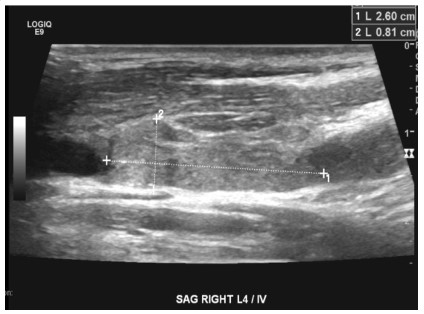
A year later after the second surgery, the patient completed
her follow up, the CT neck with contrast showed bilateral paratracheal tiny enhancing nodules at the lower thyroid bed, multiple
bilateral cervical lymph nodes and ligated partially thrombosed
RT IJV. The 123I WBS showed multiple focal area of increased uptake noted at the right side of the neck extending from right supraclavicular region to inferior border of hyoid bone (level III, IV),
while 24 hours uptake 0.17%. The US neck showed two hypoechoic nodules were noted in the right bed. in the mid bed measuring 0.7 x 0.5 x 0.3 cm and in the inferior bed measuring 0.4 x 0.3 x
0.8 cm. in addition to a few right cervical lymph nodes, suspicious
for recurrence, the largest in the right mid neck measuring 1.6 x
1.1 x 0.7 cm.
A month later, the patient had another 123I WBS and the results
showed a focus of tracer uptake localized at right thyroid bed with
24-hour uptake of 0.4% consistent with recurrent/residual soft
tissue at the thyroid bed. Also, there was a large focus of radiotracer uptake localized at the right supraclavicular region; just inferior to right thyroid bed, most likely corresponds to pathological
lymph node seen in prior ultrasound of the neck. Focal tracer activity is also noted within the suprasternal notch. There were two
foci of radiotracer uptake one seen at the posterior element of
T3 and the right iliac bone, suspicious for bone metastasis. There
was also focal increased radiotracer uptake at the anterior mediastinum with no obvious underlying structural abnormality, that
could be related to either normal thymic uptake at this age group
or -less likely- metastatic disease.
The post operative thyroglobulin level was found to have a
high risk of recurrence also, it provides incremental values to aid
the physicians in making a good decision for radioactive iodine therapy [1-3]. Although the patient had two surgeries and had a
previous radioiodine ablation therapy after the first surgery, the
patient status based on the imaging follow-up results highly recommend having a second radioiodine therapy. As known in literature, recurrence of disease in lymph nodes maybe possible post
incomplete surgical resection of neoplastic tumours and is not
prevented in all cases by postoperative radioactive iodine therapy
[4,5]. In this case, the patient had a second dose of 119 mCi which
was given orally.
A year later after the course of the second radioiodine dose,
the patient had US neck for follow-up which showed a redemonstration of new right mid thyroid bed hypoechoic fairly circumscribed minimally vascular nodule, measuring 0.3 x 0.3 x 0.5 cm.
The second right thyroid bed nodule is not visualized in the study.
Interval visualization of eight tiny hypoechoic left lower thyroid
bed nodule, measuring 0.1 x 0.1 x 0.3 cm. The bilateral lower cervical lymph nodes which demonstrate interval increase in size and
number, some of which demonstrate suspicious morphology. Findings were suspicious cervical lymphadenopathy.
Also, for follow-up the patient had 123I WBS, which showed that
there was interval resolution of most of previously seen multiple
focal tracer uptakes seen in the chest and pelvic regions related
to osseous metastasis. Subtle iodine uptake was seen in the mid
thoracic region posteriorly. There were persistent few focal tracer uptakes seen in the right neck, related to the known nodal
metastasis with interval reduction of the 24-hour calculated neck
uptake that measures about 0.17%, previously 0.4%. No new
concerning focal tracer uptake in the neck or elsewhere. The scan
shows residual iodine avid right neck nodal metastases, and probable mid thoracic spine metastatic disease. With no new focal
tracer uptake elsewhere.
In that case, physicians advised the patient to have a third
radioiodine therapy with a dose of 155.32 mCi again was given
orally.
Conclusion
The case presented illustrates a widely intensive follicular thyroid carcinoma with extensive angioinvasion. In this case, post
total thyroidectomy showed post-surgical changes both post first
and second surgery with the repetition of the radioiodine therapy
for three times. Elevation of thyroglobulin level while negative WB
scan should be kept under regular follow-up as it is a mark indicator for possible recurrent disease. Along with the medical treatment, it is important to consider the improvement of patient’s
living standards if improvements of patient’s overall life quality
besides addressing the patient’s physiological and psychological
needs, will help in focusing on prolonged survival [6,7].
Declarations
Conflict of interest: None declared.
Funding source: There were no sources of funding.
Consent: The patient had given her written consent for publication.
References
- Yang X, Liang J, Li TJ, Yang K, Liang DQ, et al. Postoperative stimulated thyroglobulin level and recurrence risk stratification in differentiated thyroid cancer. Chin Med J. 2015; 128: 1058-1064
- Mao Y, Xing M. Recent incidences and differential trends of thyroid
cancer in the USA. Endocr Relat Cancer. 2016; 23: 313-322.
- Biermann K, Biersack HJ, Sabet A, Janzen V. Alternative therapeutic
approaches in the treatment of primary and secondary dedifferentiated and medullary thyroid carcinoma. Semin Nucl Med. 2011;
41: 139-148.
- Baudin E, Schlumberger M. New therapeutic approaches for metastatic thyroid carcinoma. Lancet Oncol. 2007; 8: 148-156.
- Schlumberger M, Brose M, Elisei R, Leboulleux S, Luster M, et al.
Definition and management of radioactive iodine-refractory differentiated thyroid cancer. Lancet Diabetes Endocrinol. 2014; 2: 356-
358.
- Wu HX, Zhong H, Xu YD, Xu CP, Zhang Y, et al. Psychological and
behavioral intervention improves the quality of life and mental
health of patients suffering from differentiated thyroid cancer
treated with postoperative radioactive iodine-131. Neuropsychiatr
Dis Treat. 2016; 12: 1055-1060.
- Barbus E, Pestean C, Larg MI, Gabora K, Bonci EA, et al. Psychological impact of 131I radioprotection measures on thyroid cancer
patients. Clujul Med. 2018; 91: 441-447.