Case report
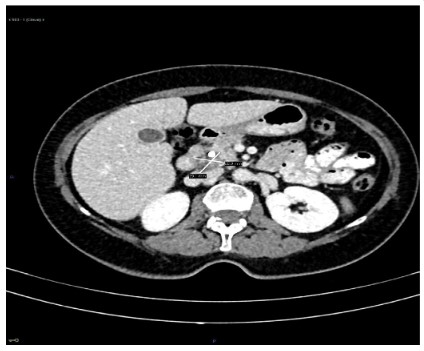
A 64-year-old woman is referred from another health center
referring epigastric pain and jaundice, caused by a lesion greater
than 2 centimeter located on the uncinate process of pancreas,
detected on an imaging test, carried out at the referral center (Figure 1). Her previous medical history included smoking habit and
hypothyroidism.
The liver function test revealed a high Total Bilirubin (TB) serum level of 5.20 mg/dl (with direct bilirubin (DB) 4.10 mg/dl and
indirect bilirubin (IB) 1.10 mg/dl); aspartate transaminase (AST)
49 U/L, alanine transaminase (ALT) 46 U/L; gamma-glutamyltransferase (GGT) 297 U/L; alkaline phosphatase (ALP) 501U/L and lactate dehydrogenase (LD) 226 U/L.
An Endoscopic Retrograde Cholangiopancreatography (ERCP)
is performed detecting a blockage over the distal portion of the
common bile duct with a biopsy sample taken, associated to an
upper gastrointestinal bleeding (UGIB) as a complication of the
procedure. Homeostasis is achieved with the endoscopic injection
of adrenaline, requiring the patient a blood transfusion.
The pathology report informed about the presence of malignancy, probably attributable to a pancreaticobiliary adenocarcinoma.
With the diagnosis, aforementioned, a cephalic pancreaticoduodenectomy (Whipple procedure) was performed, being discharged the patient at the seventh day without surgical compli-
cations. However, the patient suffered an episode of atrial fibrillation, during the post-operatory, being properly treated.
Pathological examination and Immunohistochemistry (IHC)
analysis
The pathological examination revealed a pancreas confined tumor with free resection margins, lymphovascular and perineural
invasion, and fourteen benign lymph nodes (0/14). The final diagnosis was a pancreatic carcinosarcoma.
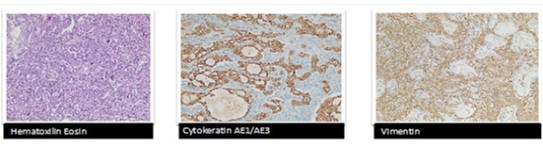
Microscopically the tumor was constituted by a morphological and inmunophenotypical components with no similarities
between them. The carcinoma component was constituted by a
moderately differentiated ductal adenocarcinoma, which express
cytokeratin AE1/AE3 and being negative for vimentin (Figure 2).
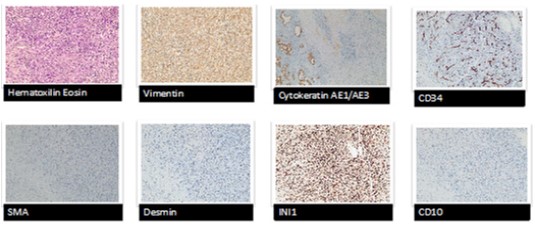
The sarcomatous component (Figure 3) was constituted by tumoral cells with a diffuse architectural pattern, a marked nuclear
atypia and pleomorphism, the presence of multinucleated giant
cells and numerous mitotic figures, with vimentin expression and
being negatives for cytokeratin AE1/AE3. There is no expression
for CD 34, smooth muscle actin and desmin, besides no angiomatous and muscular differentiation. There was not loss of INI1
expression (the loss of INI1 expression is present on the sarcomatous undifferentiated carcinoma). The CD 10 was negative, predicting a bad prognosis in case of been positive, according to experts.
During the oncological follow up the patient received adjuvant
therapy with eight cycles of Gemcitabine, and after three years
the patient is free of disease (Figure 4).
Discussion and conclusion
The collision tumors are very rare. The coincidence at the diagnosis of various tumors at a time could be frequent, being synchronous when the second primary cancer is diagnosed within 6
months of the primary cancer and metachronous when the second primary cancer is diagnosed more than 6 months after the
diagnosis of the first primary cancer. Nevertheless, a collision tumor is a neoplastic lesion comprised of two or more distinct cell
populations that maintain distinct borders.
To properly establish the histological diagnosis of carcinosarcoma, as the last WHO [1] classification guide of pancreatic tumors state, require a biphasic pattern, without a mix or transition
area, with a sarcomatous component (including or not heterologous elements) and an epithelial morphology component, which
could be an adenocarcinoma. Each component should represent
the 30% of the tumor to properly consider it as a carcinosarcoma.
Each component is inmunophenotypically similar to its typical
lineage, with a divergent expression on each component.
The sarcomatoid carcinoma should be considered on the differential diagnosis, which unlike the carcinosarcoma, is an undifferentiated carcinoma that can harbor fusiform, pleomorphic and
multinucleated giant cells, resembling the sarcoma, but lacking of
the typical biphasic pattern of the carcinosarcoma. Inmunophenotypically, could express cytokeratin AE1/AE3 and loss of INI1
expression.
Most of these tumors could be located on the uterus, but are
no often present on others organs as ovaries, breasts, lungs, prostate, urinary and digestive tracts. Those tumors diagnosed in the
pancreas are even more rare, and any publications regarding this
topic in the literature is limited [2].
The pancreas carcinosarcoma is a rare subtype of pancreatic
cancer with limited clinical and pathologic data reported in the literature with a bad prognosis [3]. It have an epithelial component
which is usually an adenocarcinoma and a sarcomatous component of fusiform cells. Each one with different inmunohistochemical and molecular features related to their differentiation lines [4].
The microscopic semblance is variable. The carcinoma component ranges from well to poorly differentiated ductal like adenocarcinoma. The sarcomatous component exhibits pleomorphic
and spindle morphologies resembling mesenchymal tumour [5].
There have been a controversy around these tumors pathogenesis from long time. The neoplastic components can develop
as two adjacent tumor lineages, so carcinoma and sarcoma collide. This could be the theory of tumoral collision. Another theory
points out to an origin sharing from a pluripotent cell that enable
the development of two different histological components [6].
The genetic predisposition, the advanced age, the environmental
carcinogens exposure, previous radiotherapy or chemotherapy
and the immunosuppression, among others, are part of the factors that increase the risk of the tumor collision [7].
Conclusion
This study shows that when epidural bupivacaine-fentanyl is administered either through intermittent or continuous method, it provides stable and comparable haemodynamic effects, sensory block height and comparable incidence of side effects for major gynaecological surgeries. We recommend that continuous and intermittent epidural anaesthesia with bupivacaine-fentanyl should be used for major gynaecological surgeries, with a preference for intermittent method as it provides more stable haemodynamic effects with lesser volume of local anaesthetic agent with fentanyl.
References
- Bosman F. Ductal adenocarcinoma variants and mixed neoplasms
of the pancreas. In World Health Organization Classification of Tumours of the Digestive System, 5th ed.; IACR Press: Lyon, France,
2019; 338-329.
- Ruess DA, Kayser C, Neubauer J, Fichtner-Feigl S, Hopt U, et al. Carcinoarcoma of the Pancreas. Case Report With Compresive Literature Review. Pancreas. 2017; 46:1225-1233.
- Alhatem A, Quinn PL, Xia W, Chokshi RJ. Pancreatic Carcinosarcoma Clinical Outcome Analysis of the Cancer Institute Database.
Journal of Surgical Researche. 2021; 259: 62-70.
- Khan J, Cheng L, House MG, Guo S. Carcinosarcoma, a rare Malignant Neoplasm of the Pancreas. Curr Oncol. 2021; 28: 5295-
5303.
- Luchini C, Pea A, Lionheart G, Mafficin A, Nottegar A, et al. Pancreatic undifferentiated carcinoma with osteoclast-like giant cells
is genetically similar to, but clinically from, conventional ductal
adenocarcinoma. J Pathol. 2017; 243: 148-154
- Li J, Wei T, Zhang J, Wei S, Chen Q, Chen BW. Carcinosarcoma of
the pancreas: comprehensive clinicopathological and molecular
characterization. HBP. 2020; 22: 1590-1595.
- Katsourakis A, Svoronos C, Chatzitheoklitos E. Carcinoarcoma of de
pancreas: how a common blood disorder can hide an extremely
rare tumour. J Pancreas. 2015; 16: 310-312.