Introduction
Since the introduction of intracavitary brachytherapy to treat
gynecologic cancer patients by Margaret Cleaves in 1903 [1,2],
vaginal cuff brachytherapy has been an effective way to deliver
ionizing radiation in endometrial cancer and selected cervical
cancer patients who are at high risk of recurrence post-hysterectomy [3]. The vaginal cuff is the upper portion of the vagina that
opens up into the peritoneum and is sutured after the removal
of the cervix and uterus during a hysterectomy. For treatment of
the vaginal cuff, the most commonly used applicator is the single-channel cylinder and two symmetric ovoid applicators according
to the shape of the vaginal stump [4]. The choice of applicator
depends on the consultant and the clinical scenario. Generally,
ovoids treat the upper part of the vaginal cuff, whereas vaginal
cylinders allow treatment of the entire length of the vagina. Both
applicators have pros and cons in clinical use and dosimetric properties. The cylinder applicator is convenient for insertion, can deliver a uniform dose distribution over the surface, and is available
in various diameters to minimize the air gap between the cylinder
and the vaginal wall. However, there is a slight underdosage to the
“dog-ear” area of the vagina [4]. The cylinder also delivers a higher dose to the bladder and rectum compared to ovoid applicators.
However, dose laterality can be modified, and the mean dose to
the rectum and bladder can be lowered by using two-ovoid applicators. However, the distance between the ovoid applicators
depends on the therapist and vaginal size, and the vaginal apex
may be underdosed with the two-ovoid technique. To overcome
the problem, we have conducted this study with three-ovoid applicators to improve insufficient dose distribution.
Materials and methods
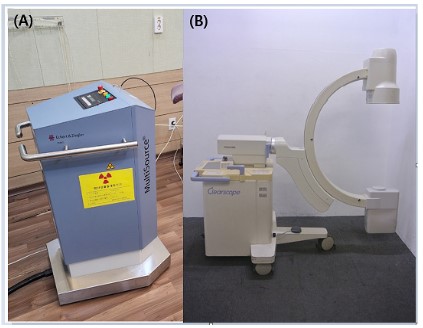
Clinical dosimetry was calculated using HDRPlus (Eckert &
Ziegler, Germany) software, and patients were treated using the
BEBIG MultiSource® High Dose Rate brachytherapy treatment unit
with a cobalt-60 source. For a treatment plan, Posterior-Anterior
(PA) projection and Right-Left (RL) lateral projection images were
acquired using the c-arm fluoroscopic x-ray system (Clear scope
SXT-9000A, Toshiba). The brachytherapy and c-arm system used
in this study are shown in Figure 1.
In this study, three types of applicators (cylinder, two-ovoid,
and three-ovoid) were used, and three brachytherapy plans were
compared for optimal dose delivery. The comparison between
various brachytherapy plans to find an optimal setting was explained to the patients, and the patients agreed to be included
in this study. The diameter of the cylinder was 3 cm, and the air
gap between the cylinder and the vaginal wall was minimized. The
two-ovoid applicators with a diameter of 1.5 cm were inserted
as symmetrically as possible in accordance with the tension and
size of the vagina. Ovoids are placed on the right and left outer
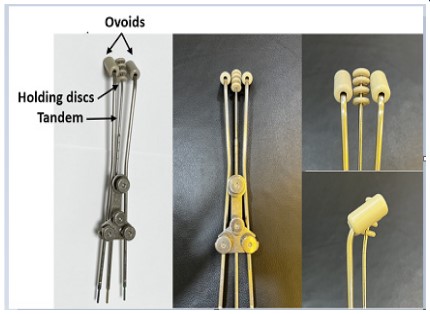
edges and the inferior side of the cervix. As shown in Figure 2, the
concept of the three-ovoid applicator was used by modifying the
fletcher-set applicator for the cervix. The three-ovoid applicator
consists of two ovoids and a tandem with multiple holding discs.
Holding discs were used to prevent perforation of the surgical site
of the vaginal cuff during insertion, and the curved direction of
the tandem was in the same direction as the ovoid. In accordance
with American Brachytherapy Society guidelines [4], the total
treatment dose was 5Gy in five separate fractions.
For each individualized treatment plan, dose optimization is
performed from a standardized plan according to the applicator
types. The aim of each plan was to provide optimal dose distributions to the prescription point, defined by a depth of 5 mm in the
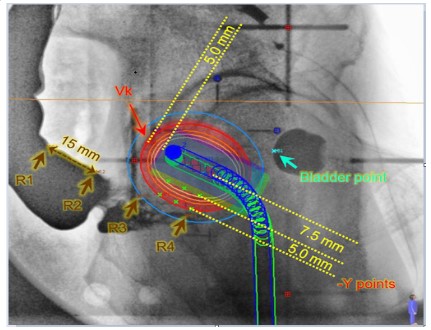
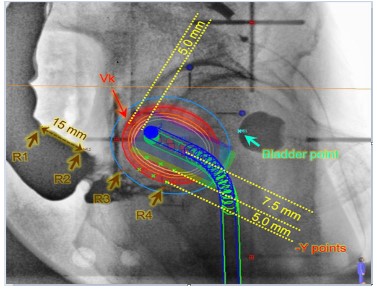
vaginal mucosa surrounding the applicator. A dosimetry analysis
was carried out using orthogonal radiographs where point doses
to critical structures were calculated according to the ICRU 38 recommendations [5]. To compare the three brachytherapy plans,
the prescription point, vaginal apex point (Vk) [6], bladder, and
rectal dose were evaluated. Figure 3 shows the schematic diagram
of the vaginal apex point and bladder and rectal dose points. The
dose at the vaginal apex point, which was defined as 5 mm above
the surface of the vaginal apex corresponding to the midline of
the applicator tips and perpendicular to the anteroposterior axis
of the patient, was calculated. In the RL image, the point located
on the back wall of the urinary balloon closest to the applicator
was marked as the bladder reference point. In addition, the barium contrast agent was used to confirm the rectal wall, and the
rectal reference point was marked along the rectal surface as the
point closest to the applicator on the rectal wall.
Results
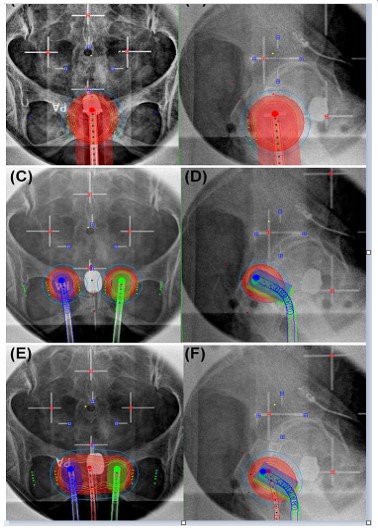
Figure 4 shows the treatment plans using the three types of
applicators, and Table 1 shows the quantitative dose assessment
results. The dose distribution was planned so that 100% of the
5Gy prescription dose could be delivered to the prescribing point.
In the plan using cylinder, two-ovoid, and three-ovoid applicators,
the calculated values for the vaginal apex point were 4.40 Gy, 2.18
Gy, and 4.68 Gy, respectively. These values correspond to 88%,
43.7%, and 93.7% of the prescribed dose, respectively. The treatment plan using the cylinder applicator showed a uniform dose
distribution overall. As shown in Figure 4C-D, the greater the distance of the two-ovoid applicators, the lower the dose appears in
the vaginal apex point. Because of some underdosing at the center of the vagina, there is a limit to delivering the dose uniformly
and conformally to the target volume. For optimal dose distribution, three-ovoid applicators are proposed to compensate for the
disadvantages of a cylinder and two-ovoid applicators. As shown
in Figure 4E-F, superior dose coverage for the vaginal cuff was obtained in the brachytherapy plan using the three-ovoid applicator.
Comparing the quantitative dose evaluation of major organs,
the bladder point doses were 3.69 Gy, 1.35 Gy, and 3.63 Gy, respectively. The rectal point doses ranged from 1.04–4.82 Gy,
1.11–2.33 Gy, and 1.89–5.33 Gy, respectively. The two-ovoid applicators delivered a lower dose to the bladder and rectum for a
given vaginal dose compared to others. The use of a cylinder and
three-ovoid applicators resulted in similar dose values to the bladder and rectum.
Discussion
In this study, three-ovoid applicators were proposed to deliver
the optimal doses to the treatment region. When deciding which
applicator to use for vaginal-cuff brachytherapy, if the “dog-ear”
area of the vagina is not present, the cylinder applicator should be
used. If there is a “dog-ear” area of the vagina, it should be simulated first with two-ovoid applicators. Currently, the greater the
distance between the two ovoids, the lower the dose appears in
the vaginal apex point. To overcome the severe cold spot, we devised a plan using three-ovoid applicators. In the two-ovoid technique, when a larger-sized ovoid is used, the dose distribution is
slightly better, but it is not completely resolved. However, three-ovoid applicators are not necessarily superior to two-ovoid applicators. If the distance between the two ovoids is not far enough
to result in a cold spot, three-ovoid applicators do not need to be
applied. Also, if there is not enough space in the intravaginal cavity, it is difficult to insert an additional ovoid between the ovoids.
Figure 5 shows a brachytherapy plan and dose distribution using the two-ovoid applicators. The prescription dose is 4Gy per
fraction, and the calculated value for the vaginal apex point is
3.27 Gy, which corresponds to 81.75% of the prescribed dose. The
bladder point dose was 1.84 Gy, and the rectal point doses along
the rectal wall ranged from 0.65–2.62 Gy, with an average dose
of 1.73 Gy. In this case, we decided to use two-ovoid applicators.
The distance between the ovoids can vary depending on the
therapist, as well as the size and tension of the vagina. If the therapist fixes the two ovoids with too much tension, it may cause
problems with the surgical suture site, so careful consideration
and experience may be required. If a severe cold spot is expected
to occur due to the distance between the ovoid applicators, even
at low tension, three-ovoid applicators may be considered.
The ultimate goal of brachytherapy is to achieve as low of radiation dose as possible to the surrounding normal tissue while
delivering the highest homogeneous dose within the target. The
main dose-limiting normal structures are the rectum and bladder, which are closer to the target in patients who have undergone hysterectomy. Therefore, rectal and bladder doses should
be minimized to reduce treatment-related side effects. Two-ovoid
applicators allow relatively low bladder and rectal doses because
of the applicator geometry while supplying reduced normal tissue doses and preventing treatment-related side effects, such
as narrow vagina and vaginal shortening. In addition, two-ovoid
applicators diminish the potential rectal injury rate [6]. However,
the mean doses to the rectum and bladder were found to be significantly higher when cylinders were used [7]. The geometry of
the cylinder applicator does not allow the optimization of rectal
dose unless shielding and multi-channel applicators [8] are used.
In this study, the highest rectal dose was shown when three-ovoid
applicators were used, while the most uniform dose was delivered to the target. Since the Vk point, rectum, and bladder are
generally located in the midline, the doses of those points have a
proportional value, although it varies depending on each applicator and the patient’s anatomy (Table 1). Because the three types
of applicators have different dose characteristics for normal organs and target doses, the selection and placement of applicators
should be made carefully, depending on the treatment scenario
and effectiveness.
There are several limitations to this study. First, although the
dosimetric characteristics were compared, we used a two-dimensional image-based brachytherapy plan. The calculated point doses may not represent the accurate dose received by the volume
of the organs. Point doses measured based on orthogonal images
sometimes lead to under or overestimating results for normal
organs. For that reason, volume-based dose calculation is better
than point dose calculation for both target and organs at risk. The
advantage of the three-dimensional image-based brachytherapy
plan is the accurate quantification of doses received by various www.journalononcology.org 4
volumes of surrounding critical structures. For more accurate
dose verification, we will apply three-dimensional image-based
brachytherapy in the future. Next, this study only proposed the
three-ovoid technique, and it is difficult to know how much the
improvement in the coverage of the Vk point affects the patient’s
prognosis. Therefore, we identified the feasibility of three-ovoid
applicators, but more patient cases and the evaluation of oncologic outcomes and toxicities are needed in further studies. Finally, since each hospital may have different applicators, it may be
difficult to broadly apply this technique. However, understanding
these concepts will enable application with little modification for
each applicator.
Table 1: Quantitative assessment for 3 types of applicators.
|
Cylinder
applicator |
Two-ovoid
applicators |
Three-ovoid
applicators |
| Prescription point dose: Left (Gy) |
5 |
5 |
5 |
| Prescription point dose: Right (Gy) |
5 |
5 |
5 |
| Vk: Vaginal apex point dose (Gy) |
4.4 |
2.18 |
4.68 |
| Bladder point dose (Gy) |
3.69 |
1.35 |
3.63 |
| Rectum point dose 1 (Gy) |
4.82 |
2.15 |
3.64 |
| Rectum point dose 2 (Gy) |
3.49 |
2.33 |
1.89 |
| Rectum point dose 3 (Gy) |
2.02 |
1.11 |
5.33 |
| Rectum point dose 4 (Gy) |
1.04 |
1.39 |
1.99 |
| Rectum: max dose (Gy) |
4.82 |
2.33 |
5.33 |
| Rectum: mean dose (Gy) |
2.84 |
1.75 |
3.21 |
Conclusion
In conclusion, according to the results of the dosimetric comparison of three types of applicators, vaginal-cuff brachytherapy
plans using three-ovoid applicators can be a way to overcome the
vaginal apex cold spot. Since the three types of applicators have
different dosimetric properties conferring specific advantages and
disadvantages for normal organs and target doses, all applicators
have good reproducibility if applicator selection and placement
are carefully made.
Declarations
Statement of Ethics: Ethics approval was not required for this
article.
Conflict of Interest Statement: No potential conflict of interest
relevant to this article was reported.
Data Availability Statement: Not applicable.
References
- Cleaves MA. Radium: With a preliminary note on radium rays in
the treatment of cancer. Med Rec. 1903; 64: 601-606.
- Aronowitz JN, Aronowitz SV, Robison RF. Classics in brachytherapy:
Margaret Cleaves introduces gynecologic brachytherapy. Brachytherapy. 2007; 6: 293-297.
- Zakem SJ, Robin TP, Smith DE, Amini A, Stokes WA, et al. Evolving
trends in the management of high-intermediate risk endometrial
cancer in the United States. Gynecol Oncol. 2019; 152: 522-527.
- Small W Jr, Beriwal S, Demanes DJ, Dusenbery KE, Eifel P, et al.
American Brachytherapy Society consensus guidelines for adjuvant vaginal cuff brachytherapy after hysterectomy. Brachytherapy. 2012; 11: 58-67.
- International Commission on Radiation Units and Measurements.
ICRU Report 38, Dose and Volume Specification for Reporting Intracavitary Therapy in Gynecology. Bethesda, MD: ICRU Publication. 1992.
- Tuncel N, Garipagaoglu M, Kizildag AU, Andic F, Toy A. Optimisation techniques in vaginal cuff brachytherapy. Br J Radiol. 2009; 82: 936-940.
- Kumar NP, Kumar A, Jayaprakash PG, Raghukumar P, James FV. Dosimetric comparison of bladder, rectal, and vaginal surface doses
between ovoids and cylinder-based vaginal brachytherapy in carcinoma of the endometrium. J Cancer Res Ther. 2018; 14: 1191-1195.
- Bahadur YA, Constantinescu C, Hassouna AH, Eltaher MM, Ghassal
NM, et al. Single versus multichannel applicator in high-dose-rate
vaginal brachytherapy optimized by inverse treatment planning. J
Contemp Brachytherapy. 2015; 6: 362-370.