Relevance
Cervical cancer (CC) is the second most common cancer among
women under 65 years of age and is the most common cause of
death from gynecological cancer worldwide. In terms of morbidity and mortality, cervical cancer ranks fourth among all cancers. In 2020, there were 604,127 new cases of cervical cancer
and 341,831 deaths worldwide. In the structure of mortality from
malignant neoplasms in women under 45 years of age, cervical
cancer occupies the first place [1]. Cervical cancer recurs after primary treatment in about 10-20% of patients with early disease
and no evidence of lymph node metastases, and up to 64-70%
of patients with lymph node metastases and/or locally advanced
disease. The recurrence rate of cervical cancer correlates with the
initial prevalence of the tumor process: the more advanced the
stage of the tumor process, the higher the likelihood of recurrence [2]. Unfortunately, treatment strategies for this category of
patients are limited to palliative management of symptoms, with
most efforts to prevent disease progression and increase survival
failing. One of the possible effective methods for the treatment of
CC relapses is stereotactic radiation therapy [3,4], which makes it
possible to deliver a radical dose of ionizing radiation non-invasively, without serious toxic complications [5]. The aim of the study
was to determine the effective possibilities of using modern radiation therapy technologies in treatment programs for recurrent
cervical cancer based on a retrospective analysis of the primary
treatment of cervical cancer.
Material and methods
A retrospective analysis of 100 cases diagnosed with cervical cancer recurrence, who received treatment at the National
Medical Research Center named after Ak. E.N. Meshalkin in the
period 2011-2022. Patients were examined in accordance with
international guidelines. Relapses and metastases were determined using additional research methods-MRI, CT, PET-CT, bone
scintigraphy, and also confirmed by morphological examination.
The age of the patients varied from 24 to 82 years, while the average age of the patients was 47.7 ± 12.5 years. Patients were included in the study group by random sequential selection. In all
cases, the diagnosis of the primary tumor was morphologically
confirmed: in 88 patients (88%) - squamous cell carcinoma, in 12 - adenocarcinoma (12%). Among this group, stage 0 - 2 (2%), stage
I - 18 patients (18%), stage II - 36 patients (36%), stage III - 43
(43%), IV - 1 (1 %).
Concomitant pathology was detected in 41 (41%).
All patients of the study group (n=100) received stereotactic
conformal radiation therapy using the ELEKTA AXESSE, using modern techniques:
1. 3D-conformal radiation therapy (3D-CRT) is a remote irradiation technology that reduces the load on healthy organs
and tissues by generating an isodose that matches the volume of radiation.
2. Intensity Modulated Radiation Therapy (IMRT) is an intensity modulated dose delivery technique at static country
angles.
3. Volume modulated irradiation (VMAT) is a radiotherapy
technique in which irradiation is carried out with the simultaneous movement of the Gantry and the MLC.
Using the active breathing control system (ABC - Active Breathing Cordinator) - a type of radiation treatment that is used to irradiate tumors of organs that are mobile during breathing. (lungs,
liver, pancreas, etc.)
Different dose limits were used for critical organs, corresponding to the following hypofractionation regimens: ROD 4-8 Gy
for 3-10 fractions. ROD and SOD were determined taking into
account the tolerance of the surrounding structures. In patients
with lung metastases, radiosurgery (SRS) was used, ROD 18 Gy
per 1 fraction.
All patients received topometric CT and MRI scans, followed by
image fusion; if necessary, PET-CT data were used. Clinical tumor
volume (CTV) was the same as for GTV. For PTV, an offset of 2-4
mm was used depending on local mobility. With metastases to
the lungs, mobility was assessed depending on the position of the
focus during maximum inspiration and expiration.
Response to treatment was assessed by clinical examination,
ultrasound and MRI of CT at 3, 6, and 12 months in the first year,
and every 6 months thereafter.
Results
We analyzed the primary methods of treatment received by
the patients of the study group. As a result, it was revealed that
the main methods of treatment were surgical (used up to stage IIa
inclusive), radiation therapy (in combination with chemotherapy),
combined methods. The most common method of treatment was
combined radiation therapy, which was used in 38 patients (38%),
only surgical treatment was received by 23 (23%), chemoradiation
therapy was performed in 19 (19%), surgery in combination with
adjuvant radiation therapy was performed in 19 (19%), chemotherapy (with palliative purpose) - in 1 patient (1%). An analysis
of the primary treatments and the time to recurrence for each of
them showed that in the case of the surgical method of treatment
(including 4 cases in combination with adjuvant chemotherapy, in
3 cases with neoadjuvant chemotherapy), relapses occurred on
average after 37, 6 months. In the case of a combination of the
surgical method with adjuvant radiation therapy, the occurrence
of relapse was noted after an average of 31.4 months, with the use
of chemoradiotherapy - after 23 months. Most likely, earlier periods of recurrence in patients treated with combined methods of
treatment are explained by the initial neglect of the disease. Analysis of the distribution of patients by stages showed that among
patients with recurrent cervical cancer in this sample, stage III was
the most common - 43 patients (43%), II - 36 patients (36%), I - 18
(18%), IV - 1 (1%). In our study, it was found that locoregional recurrences were most often determined - 50 patients (50%), local
relapses were detected - 44 patients (44%), distant - 36 patients
(36%), multiple (several localizations) - 43 (43%).
CC relapses were classified according to the time of occurrence
into 3 groups: progression (up to 6 months), early relapses (from
6 to 12 months), late relapses (more than 12 months). The most
frequent were late relapses - 65 patients (65%), early - 20 (20%),
progression - 15 (15%). Locoregional relapses of cervical cancer
occurred in early forms of relapses, and more often in late ones
(65.6% of all locoregional relapses). CC metastases most often
occurred in the late follow-up period (more than 12 months) - 68.2%. Local relapses were also observed in longer periods (60%).
The analysis of radiation reactions and complications in patients
with recurrent CC was carried out. In general, it should be noted that stereotactic radiation therapy was tolerated satisfactorily
and was carried out in all patients in the planned volume. In all
cases, radiation reactions and complications corresponded to I–II
severity, did not lead to a break in the combined treatment, and
were stopped by the appointment of symptomatic drug therapy.
Acute toxicity grade 3-4 and complications after stereotactic radiation therapy were not observed.
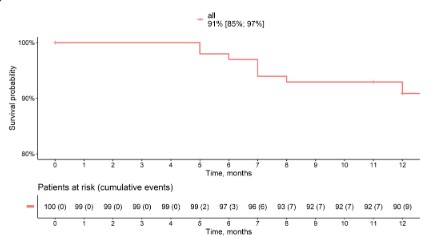
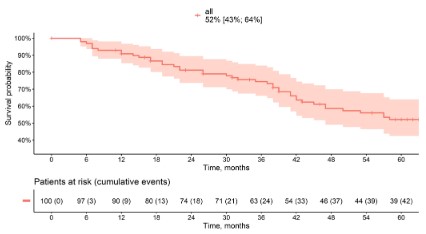
One-year mortality for patients with recurrent CC was 9% (Figure 1). Three-year survival was 74%. The five-year survival rate
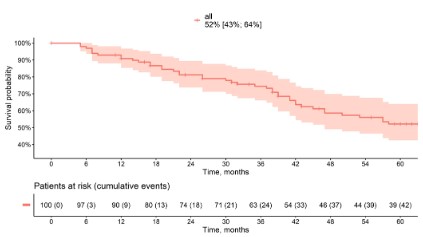
was 52% (Figure 2). Depending on the location of the recurrence,
five-year survival was 55% for the local recurrence group, 55%
for the loregional recurrence, 64% for the distant relapses, and
47% for the multiple relapses group (Figure 3). Depending on the
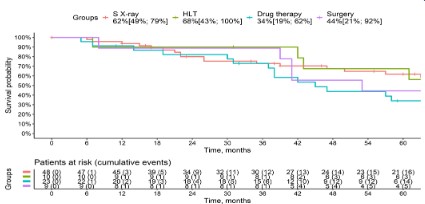
method of recurrence treatment, the five-year survival rate for
the stereotaxic radiotherapy group was 62%, for the chemoradiotherapy group, 68%, for the drug therapy group, 34%, and for the
surgical treatment group, 44% (Figure 4).
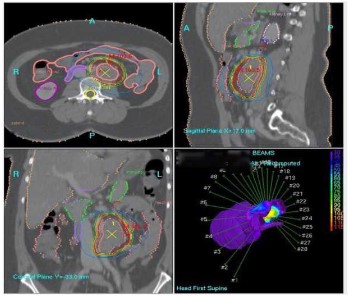
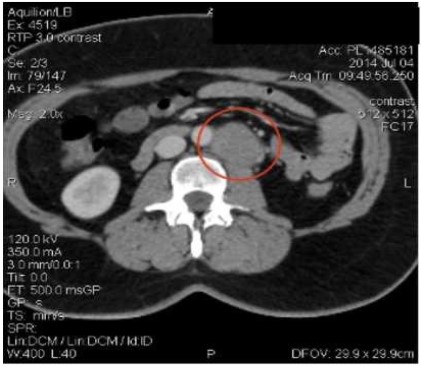
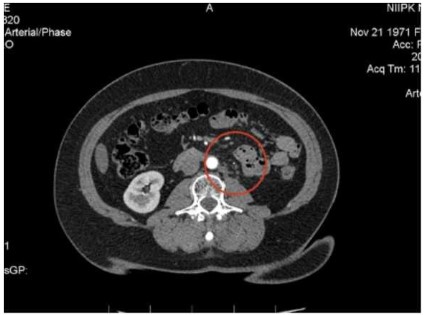
Clinical example
Patient D., 44 years old. In 2012 applied to the hospital at the
place of residence, where a separate diagnostic curettage, a knife
biopsy of the cervix was carried out, according to the result of
a histological examination of 06/04/2012, squamous cell carcinoma with keratinization with invasion of the entire thickness of
the biopsy was detected. The patient was admitted for further
examination and treatment at the Federal State Budgetary Institution Ak. E. N. Meshalkin’s with a diagnosis of stage III cervical
cancer (T1bN1M0). In August 2012 a course of combined radiation therapy was carried out a remote stage in combination with
radiomodification, then a course of intracavitary gamma therapy
using the Multisource, the Fletcher system: ROD - 5 Gy, 2 fractions per week, 6 fractions. Thus, SOD was 30 Gy, EQD2 per t.V.
= 70 Gr. EQD2 per T.A. = 80-90 Gr. In May 2014, progression was
recorded, metastases were detected in the para-aortic lymph
nodes. According to MSCT dated May 13, 2014. Conglomerates
of retroperitoneal lymph nodes up to 4 cm. Then, at the Federal State Budgetary Institution Ak. E. N. Meshalkin’s was a course
of conformal stereotaxic remote beam therapy was carried out
using the “VMAT” method (rotation with modeling according to
the intensity of irradiation), E=10 MeV, in the 5p/week mode with
irradiation of the conglomerate of retroperitoneal lymph nodes in the ROD 3 Gy to SOD 48 Gy (equivalent to SOD 60 Gy) (Figure. 5).
The treatment was carried out using IGRT image control technology. Currently, the patient has been under observation for more
than 10 years, there are no signs of recurrence of the disease, the
patient is under dispensary observation (Figure 6,7).
Discussion
The data obtained by us were analyzed in comparison with the
data of similar studies presented in the modern literature. Thus,
according to the results of the study by Perez CA et al. most often, recurrences were detected in the vaginal stump, in the small
pelvis, as well as in the form of distant metastases [8]. The most
common distant sites were para-aortic lymph nodes (81%), lungs
(21%) and supraclavicular lymph nodes (7%), the frequency of
which was associated with the stage of the disease: at stage IA
it was 0-3%, 13-16% at stage IB, 22–31% at stage IIA, 22–26% at
stage IIB, 32–39% at stage III, and 75% at stage IVA, which is absolutely comparable with our results [9,10]. It should be noted
that our study did not calculate the number of patients with CC
relapses in relation to the total number of treated CC patients,
which makes it difficult to interpret the data [11,12]. According to
M. Peiretti et al. the frequency of pelvic recurrences after radical
hysterectomy and pelvic lymphadenectomy varies depending on
the specific risk factors for each patient [13]. Patients with such
relapses after surgical treatment had a more favorable prognosis
compared with patients with relapses after the use of primary radiation therapy alone, which also coincides with our results [14].
It should be noted that our study is not without limitations due to
its retrospective nature, small sample size, and the lack of longterm results in the treatment of recurrent cervical cancer, which
indicates the need and prospects for continuing the current study
[15].
Conclusions
• Despite the early stages of the disease and the effectiveness
of treatment methods, relapses were recorded in 54% of
cases in patients with stages I (18%) and II (36%) of the disease, which confirms the need for more frequent and longterm monitoring of a group of patients with early stages of
cervical cancer.
• Local recurrences most often occurred in patients with stage
I disease (55% of cases), while locoregional recurrences
were more often detected in patients with stage III disease
(62.5%). Given this nature of recurrence, during the observation period, an examination by an oncogynecologist, colposcopy, pathomorphological examination, ultrasound of
the pelvic organs and abdominal cavity, and CT is necessary.
• The most common localizations of distant cervical cancer
metastases are bones and lungs (35.8% each), brain and liver (14.2% each). Among distant lymphogenous metastases
are inguinal and supraclavicular lymph nodes (50% each).
• Late relapses (more than 12 months) occurred in 65% of
cases, regardless of the stage of the disease, which dictates
the need for a longer follow-up of patients after treatment
with cervical cancer.
• One of the most effective methods for treating recurrent
cervical cancer is stereotaxic conformal radiation therapy;
in this sample, it was used regardless of age, stage of the
process, type of primary treatment, and results of pathomorphological examination.
Funding: This study did not require additional funding.
Conflict of interest: The authors declare no conflict of interest.
References
- Bohman Ja. V. Rukovodstvo po onkoginekologii. M.: Medicina.
1989; 463.
- Gadducci A, Cosio S. Pharmacological Treatment of Patients with
Metastatic, Recurrent or Persistent Cervical Cancer Not Amenable
by Surgery or Radiotherapy: State of Art and Perspectives of Clinical Research. Cancers (Basel).2020; 31: 75-78.
- Sovremennye podhody k vyboru taktiki lechenija u bol’nyh rakom
shejki matki / Chernyshova A.L., Kolomiec L.A., Trushhuk Ju.M. I Dr.
Opuholi zhenskoj reproduktivnoj sistemy. 2021; 17: 128-133.
- Kanao H, Aoki Y, Omi M, Nomura H, Tanigawa T, et al. Laparoscopic
pelvic exenteration and laterally extended endopelvic resection
for postradiation recurrent cervical carcinoma: Technical feasibility and short-term oncologic outcome. Gynecol Oncol. 2021; 161:
34-38.
- Krasil’nikov S. Je. Patomorfologicheskoe obosnovanie neoadjuvantnoj himio-, luchevoj terapii v sochetanii s induktorom interferonogeneza v kompleksnom lechenii raka shejki matki: dissertacija
doktora medicinskih nauk, Novosibirsk, 2004; 296.
- Kanao H, Aoki Y, Hisa T, Takeshima N. Laparoscopic laterally extended endopelvic resection (LEER) for cervical carcinoma recurring at the pelvic sidewall after concurrent chemoradiotherapy:
Our experience in three cases. Gynecol Oncol. 2018; 149: 428-429.
- Management of recurrent cervical cancer: a review of the literature. Peiretti M, Zapardiel I, Zanagnolo V Surg Oncol. 2012; 21:
e59-66.
- Marth C, Landoni F, Mahner S, McCormack M, Gonzalez-Martin A,
et al. ESMO guidelines committee cervical cancer: ESMO clinical
practice guidelines for diagnosis, treatment and follow-up. Ann.
Oncol. 2018; 29: 262.
- Cibula D, Potter R, Planchamp F, Avall-Lundqvist E, Fischerova D,
et al. The European Society of Gynaecological Oncology/European
Society for Radiotherapy and Oncology/European Society of Pathology guidelines for the management of patients with cervical
cancer. Radiother. Oncol. 2018; 127: 404-416.
- Kanao H, Aoki Y, Hisa T, Takeshima N. Total laparoscopic pelvic
exenteration for a laterally recurrent cervical carcinoma with a
vesicovaginal fistula that developed after concurrent chemoradiotherapy. Gynecol Oncol. 2017; 146: 438-439.
- Cohen AC, Roane BM, Leath CA 3rd. Novel Therapeutics for Recurrent Cervical Cancer: Moving Towards Personalized Therapy.
Drugs. 2020; 80: 217-227.
- Laliscia C, Fabrini MG, Delishaj D, Morganti R, Greco C, et al. Clinical outcomes of stereotactic body radiotherapy in oligometastatic
gynecological Cancer. Int. J. Gynecol. Cancer. 2017; 27: 396-402.
- Gadducci A, Cosio S. Pharmacological Treatment of Patients with
Metastatic, Recurrent or Persistent Cervical Cancer Not Amenable
by Surgery or Radiotherapy: State of Art and Perspectives of Clinical Research. Cancers (Basel). 2020; 12: 2678.
- Tewari KS, Sill MW, Long HJ, Huang H, Ramondetta LM, et al. Improved survival with bevacizumab in advanced cervical cancer. N.
Engl. J. Med. 2014; 370: 734-743.
- Rao D, Mallick AB, Augustine T, Daroqui C, Jiffry J, et al. Excision repair crosscomplementing group-1 (ERCC1) induction kinetics and
polymorphism are markers of inferior outcome in patients with
colorectal cancer treated with oxaliplatin. Oncotarget. 2019; 10:
5510-5522.