Introduction
Primary frontal sinus carcinoma is extremely rare, with an
incidence of 0.3-1% of all paranasal sinus carcinomas. It occurs
more often in adults over 50, mostly men [1,2]. Its symptoms are
vague and nonspecific. They can very commonly mimic different
allergology, dermatologic, or neurologic conditions making the
diagnosis hard to conclude. A CT/MRI examination in suspicious
cases is vital to the early diagnosis. Pathological examination
is needed for the definite diagnosis of primary frontal sinus
carcinoma. The predominant histological type in 39.8% of cases
is squamous cell carcinoma [3]. Treatment includes total surgical
resection followed by radio- and chemotherapy. Due to the late
diagnosis and the ability of the tumor to infiltrate into surrounding
tissues and cavities, these types of malignancies have a very poor
prognosis.
Results
We present an 84-year-old woman who, about a month ago,
developed erythema and edema of the skin of the upper eyelids
and glabella, accompanied by eye discharge and slight tenderness
to touch. We performed an X-ray and CT examination of paranasal
cavities which found no pathological changes. After consultation
with an allergologist, treatment with antihistamines was started,
but due to lack of effect, the patient was referred to the clinic
for diagnostic clarification. Additional paraclinical examinations
and specialized consultations did not confirm the suspicions
of dermatomyositis, trichinellosis, and an acute inflammatory
process. Treatment with antibiotics and corticosteroids remained
ineffective. Due to the growth of edema and the formation of a
dense lesion at the base of the nose and frontal sinus (Figures
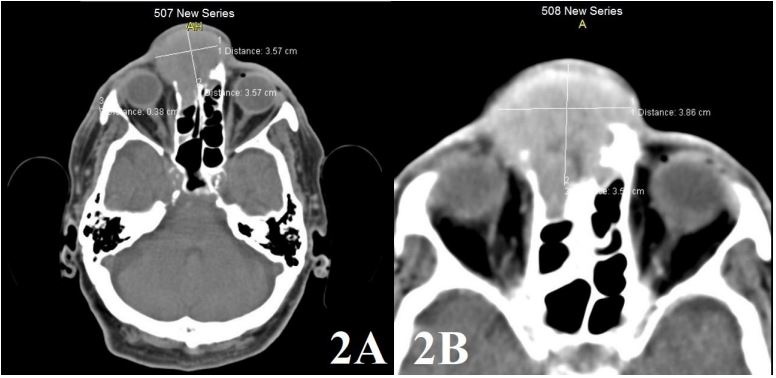
1A and 1B), a repeat CT examination of the paranasal cavities was performed, which established the presence of a soft tissue
oval lesion frontally in the area of the glabella with dimensions
of 38/36/40 mm, which infiltrates and lyses the upper part of the
right nasal bone, anterior ethmoid cells, medial wall of the right
orbit, and anterior wall of the frontal sinus (Figures 2A and 2B).
The patient was referred to an otorhinolaryngology clinic, where
a diagnosis of low-differentiated squamous cell carcinoma (NSE -
negative, p63 - positive, cytokeratin 34be12 - positive) was made
with the help of biopsy and immunohistochemical examination.
Due to the judgment of inoperability, definitive large-fractionated
percutaneous radiotherapy was performed according to a scheme
of 10x3 Gy (equivalent to 38 Gy). Due to the inoperability and lack
of good response to the performed radiotherapy the patient died
two months after therapy.
Discussion
Frontal sinus malignancies are rare and are most commonly
the result of a direct extension of the tumor from the nasal cavity
or anterior ethmoid sinuses into the frontal sinus. Primary frontal
sinus carcinomas are an extremely rare finding [4]. In 1907, Prawssud was the first to report cell carcinoma of the frontal sinus [5].
Since then, there have been multiple cases presented and in all,
we find that the initial making of the diagnosis can be challenging. The most frequent histologic types are represented by squamous
cell carcinomas (SCC, 39.8%), mature B-cell lymphomas (17.5%),
epithelial neoplasms not otherwise specified (10.5%), and Adenocarcinomas (ADC, 9.9%) [3].
The most common symptoms in primary frontal sinus carcinomas can include nasal obstruction, nasal bleeding, nasal discharge, anosmia, proptosis, diplopia, facial pain, headache, and
oppressive sensation [6]. Reddy et al. [7] also reported a case of
frontal sinus cancer mimicking acute frontal sinusitis. Edema of
the periorbital region could also be one of the initial symptoms
[8]. In the present case, the patient was initially treated for allergic sinusitis and acute inflammatory process before the diagnosis
was made. The patient was also examined for dermatomyositis
and trichinellosis which could also mimic some of the symptoms
of frontal sinus carcinomas. The unspecific early symptoms and
the rarity of the condition are the reason why these tumors are
often diagnosed at an advanced stage.
An early diagnosis usually depends on the characteristics
found upon CT/MRI examination. Evaluation of the precise extent
of frontal sinus tumors is extremely important for the surgical
approach and post-surgical treatment planning in patients. The
definite diagnosis is made with biopsy and pathological results
[9]. The present case showed mainly skin symptoms, including
erythema and edema in the upper eyelids and glabella. It is important to keep in mind the diagnosis of frontal sinus carcinoma in
patients with such symptoms, especially when they are persistent
and not responding to therapy. Early CT/MRI examination in suspicious cases can help in an earlier diagnosis and better prognosis.
The treatment of frontal sinus carcinomas includes radical surgical excision, radio- and chemotherapy. Due to the rarity of the
condition, there are no standard treatment strategies. Previous
studies show that radical resection significantly reduces the symptoms and decreases the recurrence rate. A clinical trial reported
by Guntinas-Lichius et al. [10] described the different options for
therapy in patients with perinasal tumors. The study indicated
that radical surgery is the treatment of choice for stage I-II tumors. However, due to the complicated anatomy of the frontal sinus, particularly in those patients with wide intracranial invasion,
radical surgery can sometimes be impossible. In the present case,
the reason for inoperability was the fact that the tumor infiltrates
and lyses the upper part of the right nasal bone, anterior ethmoid
cells, medial wall of the right orbit, and anterior wall of the frontal
sinus. Therefore, large-fractionated percutaneous radiotherapy
was performed. Several studies show that radiotherapy is helpful in local control of frontal sinus carcinomas which are inoperable [11]. In advanced paranasal sinus carcinomas radiotherapy
alone proved to be ineffective [12]. Currently, the combination of
chemotherapy and radiotherapy is considered to be the favored
choice.
Frontal sinus malignancies show a very poor prognosis, with a
5-year disease-specific survival of 44.2% regardless of the histology. This is due to the late diagnosis due to non-specific symptoms
and the early propensity of tumors involving this area to easily invade the orbit and the anterior cranial fossa [3]. Most of the described cases that are operable have good outcomes after surgery,
but the majority of patients don’t have satisfactory effects from
the following chemo and radiotherapy. Wang Z et al. followed 5 cases of squamous cell carcinoma and one case of osteosarcoma
all of whom underwent successful surgery. Nevertheless, the median survival time was 56 months [13]. In the presented case a
lethal exitus followed two months after therapy. Inoperable patients tend to have a lower survival rate than in general.
Conclusion
The rarity of frontal sinus carcinomas, their unspecific symptoms, and the poor prognosis make it a very complicated diagnosis. In conditions with poor prognosis and low survival rate it is
vital to make an early diagnosis. Our case highlights the need for
broad differential-diagnostic thinking in cases with edema in the
head region as it is one of the early and unspecific symptoms in
frontal sinus carcinomas.
References
- Vrionis FD, Kienstra MA, Rivera M et al. Malignant tumors of the anterior skull base. Cancer Control. 2004; 11: 144-151.
- Gerlinger I, Gobel G, Tóth E et al. Primary carcinoma of the frontal sinus: a case report and a review of literature. Eur Arch Otorhinolaryngol. 2008; 265: 593-597.
- Dutta R, Dubal PM, Svider PF, et al. Sinonasal malignancies: A population-based analysis of site-specific incidence and survival. Laryngoscope. 2015; 125: 2491-2497.
- Bhojwani A, Unsal A, Dubal PM, et al. Frontal Sinus Malignancies: A Population-Based Analysis of Incidence and Survival. Otolaryngol. Neck Surg. 2016; 154: 735-741.
- Prawssud NG. Carcinoma sinus frontalis. Vestnik Oftalmologii. 1907; 24: 253-255.
- Yoshida N, Kanekura T, Hashiguchi T, et al. Primary squamous cell carcinoma of the frontal sinus. J Dermatol. 2006; 33: 855-857.
- Reddy MS, Gihooly M, Wallace M et al. Frontal sinus carcinoma presenting as acute sinusitis. J Laryngol Otol. 1991; 105: 121-122.
- Gerlinger I, Gobel G, Toth E, et al. Primary carcinoma of the frontal sinus: a case report and a review of literature. Eur Arch Otorhinolaryngol. 2008 May; 265(5): 593-7. doi: 10.1007/s00405-007-0491-x.
- Heng-Zhu Zhang, Yu-Ping Li, Lei She, et al. Primary carcinoma of the frontal sinus with extensive intracranial invasion: A case report and review of the literature. Oncol Lett. 2014; 7(6): 1915-1918.
- Guntinas-Lichius O, Kreppel MP, Stuetzer H, et al. Single modality and multimodality treatment of nasal and paranasal sinuses cancer: A single institution experience of 229 patients. Eur J Surg Oncol. 2007; 33: 222-228.
- Rischin D, Porceddu S, Peters L, et al. Promising results with chemoradiation in patients with sinonasal undifferentiated carcinoma. Head Neck. 2004; 26: 435-441.
- Dirix P, Nuyts S, Geussens Y, et al. Malignancies of the nasal cavity and paranasal sinuses: long-term outcome with conventional or three-dimensional conformal radiotherapy. Int J Radiat Oncol Biol Phys. 2007; 69: 1042-1050.
- Wang Z, Yu J, Zhang Y, et al. Clinical Characteristics and Long-Term Outcomes following Surgery Combined with Adjuvant Radiotherapy for Patients with Frontal Sinus Malignancies. J Neurol Surg B Skull Base. 2022; 84(6): 609-615. doi: 10.1055/a-1924-9319.