Case presentations
Case 1: A 66-year-old female patient reports to a general
practitioner for a standard examination. She has no complaints
like pain and similar problems. Within the framework of a systematic examination of patients by age, a standard examination
is carried out, consisting of anamnesis and clinical examination
by organ systems, and verification of the basic laboratory and ultrasound examination of the abdomen. It is recommended in the
framework of preventive examinations and X-ray examination of
the lungs older than 65 years of age as well as screening for early
detection of tumors of the digestive tract by testing for occult
bleeding in the stool FOBT (Fecal Occult Blood Test). Women are
also given a recommendation for examination by a gynecologist
as part of preventive examinations.
The patient is not febrile. Blood pressure 120/80 mmHg, ECG
(electrocardiography), heart rate 75, normogram, no signs of
ischemia and myocardial lesions. During auscultation, vesicular
breathing is heard, without accompanying pathological phenomena. Renal lodges and abdomen painless to succus and palpation.
Palpatrono abdomen soft, peristalsis at auxsulation audible. Neurological examination of cranial nerves neat has no neurological
outbursts.
Basic laboratory analysis of urine and serum does not show
pathological values.
Urine appearance: clear; color: yellow; relative density:
pH reaction: 5 1; proteins: 0 arb.jed.; glucose: 0 arb. food; methylketones: 0 arb. jed.; urobilinogen: bilirubin: 0 arb.jed.; hemoglobin: 0 arb. nitrite: 0 arb.jed. Serum analysis: glucose: 6.0
mmol/.; urea: 8.3 mmol/; creatinine: 78 umol/L; uric acid: 301
umol/L; bilirubin-total: 14.1 umol/; Bilirubin-direct: 4.2 umol/.
iron: 11.7 umolL; AST: 34 U/L; ALT: 39 U/L; GGT: 186 U/L; cholesterol: 4.08 mmoV/L HDL-cholesterol: 2.39 mmol/; LDL-cholesterol: 1.27 mmol/; triglycerides: 0.92 mmol/L; non HDL: 1.69
mmol/L; LDL coefficient: 1.71 1; Atherosclerosis index: 0.53.
X-rays on the lungs and heart are neat. FOBT negative. A neat
patient had a hysterectomy due to uterine fibroids during menopause.
However, on ultrasound examination of the abdomen and kidneys, a change in the liver is observed.
Ultrasound examination of the abdomen: The liver is on the
shown intersections in the MKL (Medio Klavicular Line) of normal
size, with a relatively clearly limited hyphenous zone with a diameter up to 6 cm in the right lobe (differential diagnostic-zone of focal fat infiltration) - CT examination of the abdomen is proposed.
Intra and the displayed extrahepatic bile ducts are not dilated.
The cholecyst is of normal size, without calculosis and inflammation, with an apparent hyperechogenic change of diameter up to
3 mm in the region of the fundus, ultrasonic features of polyps.
The pancreas is on the displayed parts of normal size, homogeneous echostructure. Both kidneys are normal in size, maintained
the width of the parenchyma, without signs of calculosis and hydronephrosis. The spleen is on the displayed parts of normal size,
homogeneous structure. Not detected the presence of free fluid
in the abdomen.
Radiologists recommend CT (Computed Tomography) examination of the abdomen.
CT scan of the abdomen: On examination covered basal parts
of the pulmonary parenchyma, the area of pathological density
are not registered. In the pleural, as well as the pericardium, the
space does not register pathological complexion collections. The
liver is the normaine size, bilaterally present individual and poured
hypovascular changes, with the reaction of the surrounding parenchyma, and the largest total basin in S4/3, measuring 7x9x6.5
cm (APxLLCC). In the liver hilus in the cell group, there are enlarged multiplied necrotic lymphonoids, with a shorter diameter up
to about 15 mm. Intra or extrahepatic ducts are not dilated. The
cholecyst is of normal size, it is clearly contoured. The pancreas
is of normal size, clear contour, homogeneous structure, without
dilation of the main pancreatic ductus. The spleen is of normal dimensions, proper contour, homogeneous structure. The adrenals
are of orderly morphology. The kidneys are normal in size, shape
and position, have regular contours, normal parenchyma debut,
recognizable corticomedular border, without dilation of the pelvic
systems. There is no intraperitoneal and retropertoneal lymphadenogrammy. There is no free intraperitoneal fluid. Abdominaine
aorta and VCI (inferior vena cava) are of the correct position, clear
contours, normal lumen width. Bladder moderately distend, without pathological changes. Condition after hysterectomy. Zone
of sclerosis in the left aspect of the iliac bone, diameter about 10
mm, differential diagnosis corresponds to insula compacti.
The conclusion by radiologists is that there are multiple hypovascular focal lesions of the liver with signs of confluence with the reaction of the surrounding parenchyma, according to the morphological characteristics of differential diagnostic, multiple liver
abscesses (secondary deposits) come into account, but even the
primary neoplasm cannot be excluded with certainty. Necrotic
multiplied lymphnodes in the hilus of the liver. A detailed clinical/
laboratory examination is proposed, with further diagnostic evaluation if necessary.
The patient is further referred to the recommendations for
examinations in the direction of examination of oncologists and
analysis of tumor markers in order to obtain a final diagnosis and
carry out adequate treatment.
Case 2: A 71-year-old female patient reports to a general practitioner for a standard examination. It does not state that there are
any problems in my examination. Except sometimes discomfort in
the lower abdomen in the area suprapubic in the projection of
apendix but not constantly and does not associate problems with
urination or stool. She says she’s had problems going back a few
months. She did not notice a change in weight in the weight loss.
As stated in the previous case within the framework of the systematic examination of patients by age, a standard examination
is carried out, consisting of anamnesis and clinical examination
by organ systems, as well as checking the basic laboratory and
ultrasound examination of the abdomen. It is recommended to
undergo preventive examinations and X-ray examination of the
lungs over 65 years of age as well as screening for early detection
of tumors of the digestive tract by testing for occult bleeding in
the stool FOBT (fecal occult blood test). Women are also given a
recommendation for the examination of a gynecologist as part of
preventive examinations and given the problems that the patient
stated, it is especially emphasized that a gynecological examination is necessary.
The patient is not febrile. Blood pressure 130/80 mmHg, ECG
(Electrocardiography), heart rate 75, normogram, no signs of ischemia and myocardial lesions. The patient is a long-time hypertonic on adequate therapy and with regular blood pressure control
is recorded as normal. During auscultation, vesicular breathing
is heard, without accompanying pathological phenomena. Renal
lodges and abdomen painless to succus and palpation. Palpatrono
abdomen soft, when palpation in the suprapubic right and parumbilical right there is no painful sensitivity or palpatory presence of
tumeaction, peristalsis at auxulation audible. Neurological examination of cranial nerves neat has no neurological outbursts.
Basic laboratory analysis of urine and serum does not show
pathological values. Urine appearance: Clear Color: yellow, relative density: pH reaction: 5 1; proteins: 0 arb.jed.; glucose: 0 arb.
jed.; methylketones: 0 arb.jed.; urobilinogen: bilirubin: 0 arb.jed.;
Hemoglobin: 0 arb. jed. Nitrites: 0 arb jed.; Leukocytes: 1 field
of view. Serum analysis: glucose: 5.8 mmol/L; urea: 6.2 mmol/L;
creatinine: 72 umol/L; uric acid: 377 umol/L; bilirubin total: 22.1
umol/L bilirubin-direct: 4.4 umol/L; CRP: 3.2 mg/L; iron: 22.1
umol/L; sodium: 141 mmol/L potassium: 3.9 mmol/L; chlorides:
103 mmol/L; calcium: 2.50 mmol/L; inorganic phosphorus: 0.96
mmol/L; AST: 17 U/L; ALT: 18 U/L; ALP: 64 U/L; GGT: 22 U/L; alphaamylase (S): 34 U/L LDH: 150 U/L; cholesterol: 5.86 mmol/L; HDLcholesterol: 1.14 mmol/L; LDL cholesterol: 4.04 mmol/L; triglycerides: 1.49 mmol/L; non HDL: 4.72 mmol/L; LDL coefficient: 5.14 1;
atherosclerosis index: 3.54.
X-rays on the lungs and heart are neat. FOBT negative. Ultrasound examination of the abdomen and kidneys neat.
Gynecological findings
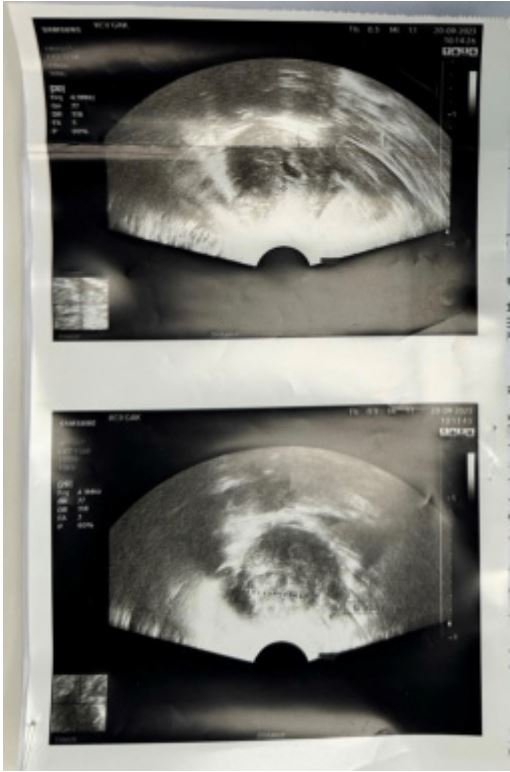
Gynecological ultrasound
The uterus in an incremental position with a smaller subserous
fibroid of the anterior wall with a diameter of 25 mm and easily
extended coffee, the possible presence of a smaller endometrious
polyp. The ovaries are not visible with a vaginal probe. While the
abdominal probe observes an oblong cystine formation significantly separated from the uterus, of open etiology. Without the
presence of free flow (Figure 1).
Based on the gynecological examination, the gynecologist advises the examination of the abdominal surgeon.
Surgeon’s findings and opinion
Patient referred by a gynecologist due to radiologically described tumor appendages. As part of the regular gynecological
examination, a change was observed on the right ovary, which
caused the patient to be sent for CT (Computed Tomography) and
then MRI (Magnetic Resonance Imaging) evaluation.
CT scan of the abdomen
Basal to the right side are visible fibrous-adhesive changes. In
the pleural, as well as the pericardial space, pathological complexions are not registered. On the posterior contour of the gastric
fundus, you can see a change in the appearance of the diverticulum of the stomach, a diameter of the neck about 14 mm, sacus
about 35 mm - for the detalinium evaluation, gastrography / gastroscopy is suggested. The liver is of normal size, regular contours,
normal ratio of the desa and left liver, homogeneous structure.
Intra-estraepation bile ducts are not dilated. The cholecyst is normal in size, it is clearly contoured. The pancreas is normaine in
size, clear contour, homogeneous structure, without dilation of
the main pancreatin ductus. The spleen is of normal dimensions,
proper contour, homogeneous structure.
The adrenals are of orderly morphology. The kidneys are normaine in size, shape and position, have regular contours, normal
thickness of the parenchyma, recognizable corticomedal border,
without dilation of the cartilage systems. Several corticaine microcysts are bilaterally present, one parenchymal cyst of the right
kidney with a diameter of 6mm can be seen. The pyelocal system of the right kidney is extrarenally laid. There is no intraperitoneal and retroperitoneal lymphadenogrammy. There is no free
intraperitoneal fluid. The abdominal aorta (marginal sclerotiona)
and VCI (Inferior Vena Cava) are of correct position, jane contour,
normal lumen width. The urinary bladder is dislocated, without
rough pathological changes. The uterus in the AVF (Ante Versio
Flexia), in the anterior aspect of the uterus is occupyed by myoma
djametra about 25 mm, which lies on the roof of the bladder; another change in similar characteristics suspect and in the region of
the left lateral wall of the corpus, 21 mm in diameter. In the projection to the right adnex interposed with the surrounding intestinal meanders, oblong, cystic change 55x34x27 mm (AP,LL,CC),
with internal septs. It is necessary an MRI of the pelvis. The right
urethra is free, the left is not entirely filled with contrast to the
delayed study (probably due to peristaltic wave). Left adnexa inconspicuous. The presence of free tenness is not registered in the
pelvis. In the inguinums bilaterally present individual lipomatous,
non-signifificant lymphonoids. By examining the covered bone
structure without infiltration.
Conclusion of the radiologist’s findings
Changes in the appearance of uterine fibroids. Cystic promeria
in the projection of the right adnex - it is necessary to make an
MRI of the pelvis for a definitive diagnosis
MRI examination: Described in the region of the right adnex
oblong, cyst lesion sized approximate dimensions 54x34x60 mm
with present internal septas that postcontrast reinforce IS; suspected existence of two smaller soft tissue thickenings on posterior wall up to 4 mm in diameter. The described change is in
close contact with the denim ovary, which has been atrophically
altered with two small retention cysts, but one gets the impression that romena in the prom order of origin of the appendages,
less likely ovaries. The patient reports occasional pain in the ileocecal region, but that she did not have problems associated with bowel movements, nor the appearance of blood in the stool. It is
proposed to make a colonoscopy and tumor markers (CEA (Carcinoembryonic marker), CA (Colon Tumor marker) 19.9) for a definitive diagnosis. A colonoscopy is also suggested. All additional
diagnostic tests are to establish a final diagnosis and to exclude a
possible diagnosis of cancer.
Discussion
According to literature and data, the number of people aged
80 or older is expected to increase significantly by 2050, from 143
million in 2019 to 426 million by 2050. This trend is due to the
ageing population and population growth. Cancer treatment in
the oldest patients can be challenging due to the high level of
comorbidity, weakness and limited life expectancy that characterizes this age group. Excluding those over 65 years of age from
clinical trials, along with high heterogeneity in a health condition
among the oldest, contributes to deficiency or overtreatment. As
a result, the survival of patients in this age group is the lowest
compared to other age groups [1,2].
The burden on cancer in Europe is on the rise, largely due to
the aging population. Between 1995 and 2018, the number of
newly diagnosed cancer cases in a sample of 31 European countries increased by about 50%, while cancer mortality increased by
about 20%. However, the number of deaths in people under the
age of 65 has decreased. Without population growth and aging,
the incidence of cancer would continue to rise, while mortality
would decrease. This is the result of an improvement in patient
outcomes, as shown by analyses of five-year survival rates, which
showed improvement in many types of cancer in Europe between
1995 and 2014 [3-5].
Adults 65 years of age or older have a 16 times higher risk of
dying from cancer compared to younger populations. The American Cancer Society, the U.S. Preventive Services Task Force, and
the Canadian Preventive Health Care Task Force offer screening
guidelines for breast, cervical, colorectal, and prostate cancers.
Recommendations are individualized based on age, life expectancy, risks, benefits and values of patients. The general consensus is
that screening with mammograms is unlikely to benefit women
with a life expectancy of less than 5 years, while screening with
colonoscopy is not recommended for those over 85 years of age.
Recently, the Canadian Working Group recommended against
colonoscopy screening at any age, supporting Fecal Occult Blood
Tests (FOBT) every 2 years and sigmoidoscopy every 10 years from
50 to 74 years of age. Discussing screening, with consideration of
patient values and reviewing potential risks and benefits, is key
to optimal patient-centered care [6,7]. Primary care physicians
may use preventive health visits or opportunistic counseling and
screening during patient encounters. In Canada, cancer screening
guidelines vary in age, tests and intervals, but most recommend
a Fecal Occult Blood Test (FOBT) or fecal immunochemical test
every 2 years for adults aged 50 to 75. The Canadian Association
of Gastroenterologists recommends similar methods, but without
recommending colonoscopy due to lack of evidence and resources. Updated guidelines for colon cancer screening are envisaged,
including diet and lifestyle as part of a risk assessment [8].
A general/family physician plays a key role in implementing
preventive measures due to close contact with citizens and the
local community as well as a role in providing preventive medical care to elderly patients, but taking into account the practical benefits of preventive measures for all elderly patients can be a challenge. When considering preventive interventions, family physicians can take into account age, life expectancy, comorbidities
and functional status, and assess the risks and benefits of screening or treatment, while respecting the values and preferences of
the patients themselves. The success of these measures is measured by preserved years of life, quality of life and reduced health
care costs. Preventive medicine aims to prevent disease and preserve health and is carried out through various procedures to prevent death, disability, impairment and decrease in quality of life.
Regular visits to the general practitioner allow early detection of
diseases and the implementation of preventive activities, which
contributes to improving health and reducing the cost of health
care [6,9]. Screening for early detection of colorectal cancer using
FOBT test, early detection of breast tumors by mammography, gynecological examination, X-ray imaging of the lungs by Low-Dose
Computerized Examination (LDCT), etc. is also recurrent in the Republic of Serbia on the basis of the rulebook by which preventive
examinations are disputed between the ages of 50 and 74 [10].
In both cases, the patients reported to the standard examination in the general practice office without specific problems.
However, a detailed examination and additional diagnostic procedures showed pathological changes that require further evaluation and treatment. In the first case, a 66-year-old patient, the
initial examination did not indicate the presence of a problem,
but an ultrasound examination of the abdomen revealed a change
in the liver. After a CT scan, multiple hypovascular focal lesions
of the liver were identified, with suspected abscesses or secondary deposits, but the primary neoplasm could not be ruled out either. Also, enlarged lymph nodes in the hilus of the liver were observed. These findings are accompanied by recommendations for
further clinical laboratory treatment and possibly additional diagnostic procedures to make a final diagnosis. In the second case, a
71-year-old patient had occasional discomfort in the lower abdomen. Ultrasound examination did not show pathological changes,
but a gynecological examination identified subserous myoma
and a suspicious cyst on the right ovary. CT and MRI scans further characterized these changes, but additional testing, including
colonoscopy and tumor marker analysis, is needed to rule out a
possible diagnosis of cancer. Both cases highlight the importance
of systematic examinations and additional diagnostic procedures
in the early detection of potentially serious diseases [10]. Following recommendations for further examination and treatment by
specialists is key to managing the health of these patients.
Conclusion
This paper discusses the important issue of the expected increase in the number of elderly people, which will have a significant impact on the health care system in the coming decades.
The aging population and population growth contribute to an increase in the burden of cancer, especially in the oldest patients.
Cancer treatment in this age group is challenging due to its high
level of comorbidity, weakness and limited life expectancy. The
lack of inclusion of elderly people in clinical trials, along with the
heterogeneity of their health condition, can lead to deficiency or
overtreatment, which can adversely affect their survival. In addition, cancer screening guidelines were discussed, which are
individualized based on age, life expectancy, risks, benefits and values of patients. It is important that the discussion of screening is conducted with patients in order to take into account their views and preferences. Family physicians play a key role in the
implementation of preventive measures in elderly patients, but
it is important to take into account the practical benefits of these
measures for each individual. Monitoring screening guidelines
and timely detection of potential illnesses is key to preserving
the health of the elderly and reducing overall healthcare costs.
Through the presented clinical experience, the importance of systematic examinations and additional diagnostic procedures in the
early detection of serious diseases in the elderly was emphasized.
Following the recommendations of specialists for further examination and treatment is crucial to effectively managing the health
of these patients.
Declarations
Conflicts of interest: Payment/services info: author have declared that no financial support was received from any organization for the submitted work.
Financial relationships: Author declared that they have no financial relationships at present or within the previous three years
with any organizations that might have an interest in the submitted work.
Other relationships: Author declared that there are no other
relationships or activities that could appear to have influenced
the submitted work.
References
- American Cancer Society. Cancer Facts & Figures 2020. Atlanta: American Cancer Society. 2020.
- Pilleron S, Soto-Perez‐de-Celis E, Vignat J, Ferlay J, Soerjomataram I, et al. Estimated global cancer incidence in the oldest adults in 2018 and projections to 2050. International Journal of Cancer. 2021; 148(3): 601-8.
- Hofmarcher T, Lindgren P, Wilking N, Jönsson B. The cost of cancer in Europe 2018. European Journal of Cancer. 2020; 129: 41-9.
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020 CA: a cancer journal for clinicians. 2020; 70(1): 7-30.
- World Health Organization. Cancer. 2020. https://www.who.int/news-room/fact-sheets/detail/cancer
- Tazkarji B, Lam R, Lee S, Meiyappan S. Approach to preventive care in the elderly. Canadian Family Physician. 2016; 62(9): 717-21.
- Mihor A, Tomsic S, Zagar T, Lokar K, Zadnik V. Socioeconomic inequalities in cancer incidence in Europe: A comprehensive review of population-based epidemiological studies. Radiology and oncology. 2020; 54(1): 1-3.
- Shimizu T, Bouchard M, Mavriplis C. Update on age-appropriate preventive measures and screening for Canadian primary care providers. Canadian Family Physician. 2016; 62(2): 131-8.
- Đurđek I. Preventive activities in the doctor’s office. Doctoral dissertation, University of Zagreb. School of Medicine. Department of Family Medicine.
- Republic Fund for Health Insurance. 2024. https://www.rfzo.rs/download/zakoni/zzo%20od%203.4.2019.pdf.